Session Information
Date: Monday, November 6, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Psoriasis is a complex disorder with cutaneous and rheumatological manifestations affecting 2-3% of the population of the Western world. The prevalence of hypertension (HTN) in patients with psoriasis has been well documented; about 30% of all psoriatic arthritis (PsA) patients have HTN. Treatment of PsA has also been shown to improve certain cardiovascular risks. We hypothesized that blood pressure was related to PsA disease activity. We also evaluated the relationship between PsA and blood pressure as it relates to initiation of TNF inhibitors (TNFi).
Methods:
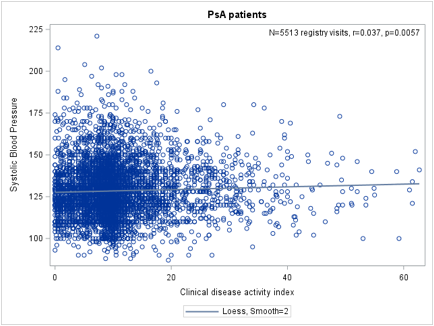
We utilized the CORRONA database and examined patients with PsA from March 2013 to January 2017. Descriptive statistics were used to summarize patient demographic and clinical data at baseline (first visit in CORRONA database). An analysis of variance was made to determine associations between 3 categories of MD-defined psoriatic body surface area (BSA) and systolic blood pressure (SBP) and diastolic blood pressure (DBP). Spearman correlations were made between continuous values of systolic or diastolic blood pressure and BSA and clinical disease activity index (CDAI) using all visits. We also looked at changes in SBP or DBP between visits correlated with changes in CDAI in those who were initiated on TNFi while they were in the registry. LOESS curves were generated to visualize relationships between variables.
Results:
1481 patients with PsA were identified, who had a total of 6109 registry visits. When body surface area (BSA) of psoriasis was categorized into ² 2%, 3-10% and >10% in analysis of variance, SBP was higher with increased BSA (p=0.0048, F=7.26, r2=0.025). DBP was also higher with an increased BSA (p<0.0001, F=15.28, r2=0.005). SBP was positively correlated with CDAI (p=0.0057, r=0.037), as was DBP (p=0.0012, r=0.044). The association between SBP change and CDAI change in those who were initiated with a TNFi showed an overall decrease in SBP that was not statistically significant (p=0.26, r= -0.041). In addition, DBP change and CDAI change in those who initiated a TNFi also showed a non-statistically significant decrease (p=0.13, r= -0.054).
Conclusion:
In patients with PsA, there was a significant positive relationship between blood pressure and both psoriasis BSA and joint disease activity, measured by CDAI. We also conclude that clinically, the initiation of TNFi did decrease blood pressure, but the decrease was not significant. We believe that this is the first study to look at relationships between the initiation of TNFi treatment and blood pressure in PsA patients.
To cite this abstract in AMA style:
Bhatt BD, Palmer JL, Curtis JR, Velkuru S, Kremer J. Changes in Blood Pressure with TNF Inhibitors for Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/changes-in-blood-pressure-with-tnf-inhibitors-for-psoriatic-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-blood-pressure-with-tnf-inhibitors-for-psoriatic-arthritis/