Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Smoking predicts higher incidence, greater severity, and reduced treatment responses in rheumatoid arthritis, lupus, and spondyloarthritis. However, cessation advice and quit line referral occur in just 10% and 0.6% of rheumatology visits, respectively. Primary care staff protocols improve guideline-based care, and electronic referrals increase use of free, state tobacco quit lines by 13-fold. We sought to examine a similar staff protocol in rheumatology using electronic health record (EHR) tools to connect eligible patients to a free, state quit line.
Methods: We conducted a pre- post-analysis of EHR data (2012-16) including our 6-month Quit Connect project. During implementation, cessation experts and project staff provided an hour of Quit Connect protocol training to nurses and medical assistants at three rheumatology clinics. The protocol included EHR prompts to assess smoking status, 30-day readiness to quit or cut back, and willingness to try a quit line. EHR data measured process steps. Referral to the quit line (vs. our published baseline) was the primary outcome. The quit line reported patient outcomes. The IRB exempted this as standard of care with permission to publish.
Logistic regression models examined process measures and referrals pre- and post-protocol. Multivariable process models included age, sex, race, body mass index (BMI), socioeconomic status (SES; defined as ever receiving Medicaid), and comorbidity (Johns Hopkins Adjusted Clinical Groups (ACG) score).
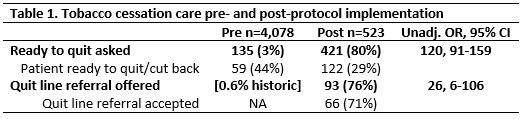
Results: For 54,090 rheumatology visits, 4,601 (9%) reported current smoking. 4,078 pre-protocol visits with patients who smoke (2012-15) were compared to 523 visits after protocol implementation (2016). Documenting smoking status remained high (96 v. 97%). 30-day readiness to quit assessment rose from 3% to 80% post-protocol (Table 1, OR 120, 91-159). Among those asked, 29% reported being ready to quit. Of those ready, 76% had a referral to the state tobacco quit line compared to our pre- rate of 0.6% (OR 26, 6-106). When offered, 71% accepted referrals (54% of ready to quit; 13% of smokers).
Patients with higher comorbidity were less often ready to quit (ACG OR 0.6, 0.4-0.9 unadj.); older patients accepted fewer referrals (OR 0.8, 0.7-0.97 unadj. per 10 yrs.). Adjusted models did not change results.
Among 66 referred patients, 11 (17%) accepted counselling, nicotine replacement, and set a quit date, and 5 more reported a quit in process. Overall, 24% of referred patients set a quit date or reported a quit attempt.
Conclusion: Our Quit Connect protocol for rheumatology staff increased quit line referrals over 20-fold. When asked, a third of patients were ready to quit and half agreed to referral. Given the importance of cessation to reduce immune and cardiopulmonary disease, future rheumatology studies should investigate cessation protocols to leverage quit lines, which are free in all states.
To cite this abstract in AMA style:
Bartels CM, Ramly E, Panyard D, Lauver D, Johnson H, Li Z, Sampene E, Piper M, McBride P. Rheumatology Clinic Smoking Cessation Protocol Markedly Increases Quit Line Referrals [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/rheumatology-clinic-smoking-cessation-protocol-markedly-increases-quit-line-referrals/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatology-clinic-smoking-cessation-protocol-markedly-increases-quit-line-referrals/