Session Information
Date: Sunday, November 5, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Reliably detecting radiographic structural change in patients with axial spondyloarthritis (axSpA), especially in the sacroiliac joints (SIJ), is notoriously difficult. Magnetic resonance imaging (MRI) is an alternative for radiographs to assess structural damage. However, so far the utility of MRI in capturing change in structural damage over time has been poorly studied. We aimed to evaluate the change over time of structural lesions on MRI of the SIJ and spine in patients with axSpA.
Methods: Patients with recent onset (≤3 years) axSpA (according to the treating rheumatologist) from the DESIR cohort were included. MRI of the SIJ (MRI-SIJ) and spine (MRI-spine) were obtained at baseline and 5 years and scored by 3 trained central readers unaware of their chronology. Structural damage in the SIJ (MRI-SIJ-STR) and in the spine (MRI-spine-STR) was defined according to 3 binary rules (A1: ≥ 5 fatty lesions and / or erosions; B1: ≥ 3 erosions; and C1: ≥ 3 fatty lesions) and 3 continuous scores (A2: number of fatty lesions /erosions; B2: number of erosions; and C2: number of fatty lesions). For binary outcomes, structural damage was defined by the agreement of at least 2 out of 3 readers and the % of net progression by subtracting the number of patients that ‘improved’ from those that ‘worsened’ divided by the total number of patients with complete baseline and 5-year data. For continuous outcomes, the mean of the 3 readers was used and the difference between year 5 and baseline was calculated.
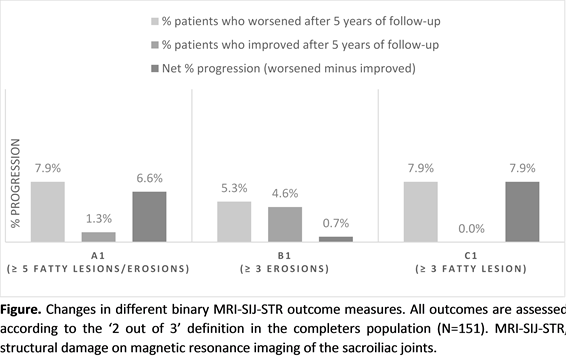
Results: In total, 151 and 145 patients had complete MRI-SIJ and MRI-spine data available from 3 readers, respectively. The percentages of net progression at SIJ level are summarized in the figure. These were 6.6%, 0.7% and 7.9% for the binary outcomes A1, B1 and C1 respectively. Notably, the percentage of ‘improvement’ (4.6%) was almost as high as the percentage of ‘worsening’ (5.3%) for definition B1 (≥3 erosions); while no ‘improvements’ were seen by the 3 readers for definition C1 (≥3 fatty lesions). Similar differences were seen for the mean (standard deviation) change of the 3 MRI-SIJ-STR continuous outcomes (A2: 1.02 (2.60); B2: 0.20 (1.39); and C2: 0.83 (2.20); p<0.01 for all). MRI-spine-STR net change over time was almost absent (A1: -0.7%; B1: 0.0%; C1: 0.7%) considering the binary outcomes, and small (though statistically significant) considering definition A2 (0.18 (0.52); p<0.01) and C2 (0.14 (0.48); p<0.01) but absent for definition B2 (0.03 (0.24); p=0.109).
Conclusion: These results suggest that patients with early axSpA only show modest structural progression in the MRI of the SIJ and that fatty lesions are more sensitive to change compared to erosions. In this early axSpA population, MRI-detected structural progression in the spine is very limited/absent.
To cite this abstract in AMA style:
Sepriano A, Ramiro S, Landewé RBM, Dougados M, van der Heijde D. Progression of Structural Damage on MRI in Patients with Axial Spondyloarthritis Is Limited: The 5 –Year Results in the DESIR Cohort [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/progression-of-structural-damage-on-mri-in-patients-with-axial-spondyloarthritis-is-limited-the-5-year-results-in-the-desir-cohort/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/progression-of-structural-damage-on-mri-in-patients-with-axial-spondyloarthritis-is-limited-the-5-year-results-in-the-desir-cohort/