Session Information
Date: Sunday, November 5, 2017
Title: Osteoporosis and Metabolic Bone Disease – Clinical Aspects and Pathogenesis Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporotic fractures are associated with high morbidity and mortality. Persons with rheumatoid arthritis (RA) have twice the risk of osteoporosis-related fracture than age-matched controls. It is not known, however, which characteristics of RA or its treatments have the greatest impact on bone mineral density (BMD). We investigated associations of RA characteristics, medication use, and body composition to low BMD in patients with RA.
Methods: We performed a cross-sectional analysis of an existing longitudinal RA cohort study from years 2007-2009. All patients met ACR classification criteria for RA. Demographic, clinical, laboratory and functional variables were collected at study visits. Body composition (fat, lean muscle and BMD) was measured by dual x-ray absorptiometry. We used linear regression to evaluate the association between predictors and femoral neck BMD. To identify independent predictors of BMD, we performed multivariable linear regression analyses that included variables significant in the univariable analyses at p<0.10. To determine if there was a linear trend between anti-cyclic citrullinated peptide (CCP) level and BMD, we repeated the linear regression analysis restricted to anti-CCP positive participants.
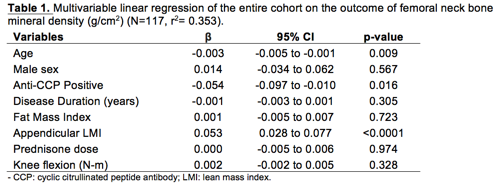
Results: Of the 138 participants (82 women, 56 men), 70% were rheumatoid factor positive, and 55% were anti-CCP positive to a level 3 times the upper limit of normal. Mean disease duration was 19±10.9 years. 44% of participants reported taking prednisone and of those taking prednisone, the mean dose was 7.1±6.1 mg/day. The mean body mass index (BMI) was 27.2±6.0 kg/m2, and mean appendicular lean mass index (ALMI) was 6.4±1.2 kg/m2; 59% of the participants were obese based on percent total body fat. 52% had low BMD based on a T or Z score <=-1 and 27% reported taking osteoporosis medications. Age and anti-CCP positivity were negatively associated with BMD, even after controlling for other variables (β=-0.003 and -0.055, respectively, p<0.05) (Table). ALMI had an independent positive association with BMD (β=0.053, p <0.0001). Among anti-CCP positive participants (n=61), higher anti-CCP level was associated with lower BMD (β for each 20-unit increase in anti-CCP=-0.011, p=0.026) when controlling for age, sex, disease duration, ALMI and knee flexion strength.
Conclusion: Anti-CCP positivity, ALMI and age were independently associated with BMD in patients with RA. The linear relationship of anti-CCP levels with lower BMD supports the hypothesis that processes specific to RA negatively impact BMD. In contrast, ALMI was positively associated with BMD, emphasizing the role of muscle mass as a potentially modifiable risk factor. Our findings highlight the complicated interplay of RA disease-specific and functional factors and their impact on bone mass.
To cite this abstract in AMA style:
Wysham KD, Shoback DM, Jafri K, Patterson SL, Schmajuk G, Imboden JB Jr., Katz PP. Association of Anti-Cyclic Citrullinated Peptide Seropositivity and Lean Mass Index with Low Bone Mineral Density in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/association-of-anti-cyclic-citrullinated-peptide-seropositivity-and-lean-mass-index-with-low-bone-mineral-density-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-anti-cyclic-citrullinated-peptide-seropositivity-and-lean-mass-index-with-low-bone-mineral-density-in-patients-with-rheumatoid-arthritis/