Session Information
Date: Tuesday, November 15, 2016
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment - Poster III: Biomarkers and Nephritis
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by the production of autoantibodies against nucleic acids and a variety of self-antigens. Recent work indicates that immune complexes containing anti-U1 Ribonucleoprotein (anti-RNP) can drive formation of neutrophil extracellular traps, which in turn can drive interferon-α production by plasmacytoid dendritic cells. (1) We hypothesized that patients with anti-RNP may be more likely to exhibit a specific pattern of SLE disease features, potentially implicating neutrophils in the pathogenesis of those features.
Methods: Clinical data from 160 patients enrolled in the FLARE cohort of SLE patients at Hospital for Special Surgery were reviewed in a retrospective fashion. All patients had been tested for anti-Ro, anti-La, anti-Sm, and anti-RNP at the time of enrollment, and patients were classified as being positive or negative for anti-RNP, whether alone or in combination with other autoantibodies. Each patient’s record was reviewed and the presence or absence of a total of 90 disease manifestations and laboratory features at any point in their history were recorded. Differences in the incidence of various phenotypes in different groups were compared between groups using Chi square tests. P values were not adjusted for multiple comparisons in this exploratory analysis.
Results: We identified 83 patients who were positive for anti-RNP antibodies (anti-RNP+), and 77 patients who were anti-RNP negative (anti-RNP(-)). We identified several disease features that differed between anti-RNP+ and anti-RNP(-) patients (Table 1). Specifically, some features classically associated with mixed connective tissue disease were seen more commonly in the RNP+ patients, such as sclerodactyly and myositis. Additionally, a history of vasculitis or elevated serum globulin (>3.5g/dL) were observed more commonly in the anti-RNP+ group. In contrast, anti-RNP(-) patients were more likely to have had a history of immune thrombocytopenic purpura or thrombocytopenia. While there was no significant difference in the prevalence of nephritis overall between the groups, membranous (class V) nephritis was more common in the anti-RNP+ patients, while proliferative (class III/IV) nephritis was more common in the anti-RNP(-) patients.
Conclusion: We demonstrated several disease manifestations which were more likely to be occur in anti-RNP+ individuals, such as vasculitis and membranous nephritis, as well as some which were more likely in anti-RNP(-) patients, such as proliferative nephritis and thrombocytopenia. The role of neutrophil activation and anti-RNP antibodies in these specific disease manifestations merits further investigation. 1. Garcia-Romo, G.S. et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci. Transl. Med. 3, 73ra20 (2011). 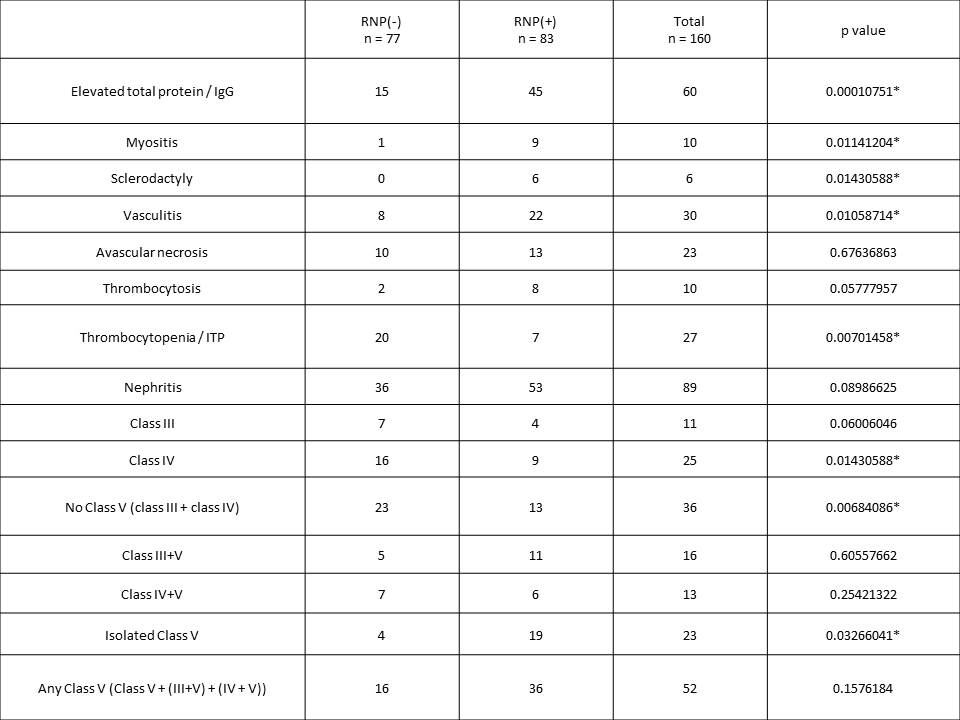
To cite this abstract in AMA style:
Fernandez D, Olferiev M, Khalili L, Kirou KA, Crow MK. Systemic Lupus Erythematosus Patients with Antibodies Against U1-Ribonucleoprotein Exhibit a Specific Pattern of Disease Manifestations [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/systemic-lupus-erythematosus-patients-with-antibodies-against-u1-ribonucleoprotein-exhibit-a-specific-pattern-of-disease-manifestations/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-lupus-erythematosus-patients-with-antibodies-against-u1-ribonucleoprotein-exhibit-a-specific-pattern-of-disease-manifestations/
