Session Information
Date: Tuesday, November 15, 2016
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment - Poster III: Biomarkers and Nephritis
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The diagnosis of Neuropsychiatric Events (NPE) in SLE is challenging and it is mainly based on the physician judgment. Structural brain imaging has limited utility in the assessment of NPE. We aimed to evaluate the utility of Brain perfusion Single Photon Emission Computed Tomography (SPECT), as a functional imaging, in the assessment of NPE.
Methods: This is a retrospective analysis on data from a single lupus centre. First, all SPECT done at the centre were identified. Second, we determined if the patients had an NPE (as determined by the physician) at the time corresponding to each SPECT. SPECT results were dichotomized as abnormal (hypoperfusion) or normal. Brain anatomical location (frontal, parietal, or others or multiple [4 or more locations]) and laterality (right, left or bilateral) of the SPECT findings were extracted. NPE were divided into focal (seizure, stroke, subarachnoid hemorrhage, aseptic meningitis [AM] or cranial neuropathy [CN]) and diffuse (organic brain syndrome [OBS], psychosis and headache). Patient weighted Sensitivity (Sn), specificity (Sp), Positive Likelihood Ratio (PLR) and Negative Likelihood Ratio (NLR) of the SPECT were determined. LR of 0.5-1 means minimal decrease, 1 no change, 1-2 minimal increase, 2-5 small increase, 5-10 moderate increase and >10 large increase in the likelihood of disease.
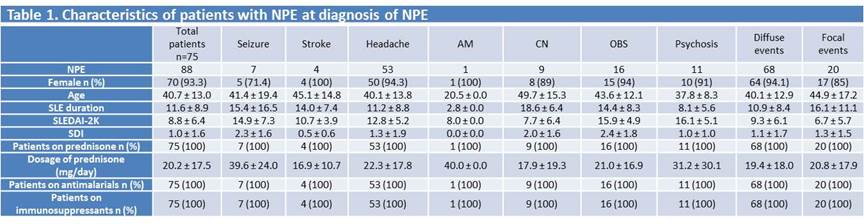
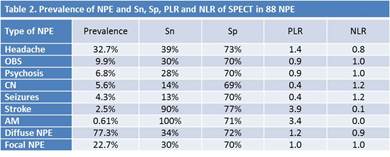
Results: 336 SPECT in 162 patients (46% patients had at least one NPE) were identified. 120 (35.7%) SPECT in 75 patients were abnormal (hypoperfusion). Of 75 patients, 93% were females, 68% Caucasian, 13% Black, 12% Asian, and 7% other ethnicities. Of the 88 NPE, 94.1% were diffuse and 26.7% were focal (Table 1). The prevalence of individual NPE on the basis of physician definitive diagnosis was 32.7% for headache 9.9% for OBS, 6.8% for psychosis, 5.6% for cranial neuropathy, 4.3% for seizures, 2.5% for stroke and 0.6% for aseptic meningitis. In diffuse NPE, the most commonly affected localizations of the SPECT hypoperfusion were the temporal lobe (18.8%) on the right side (31.5%). In focal NPE, the most commonly affected localizations of the SPECT hypoperfusion were the fronto-parietal (22.2%), temporal (22.2%) and bilateral (44.4%). Among the 3 most prevalent NPE (headache, OBS and psychosis), SPECT was useful only for headache (PLR 1.4, NLR 0.8). For headache, first, the decision to perform a SPECT should be driven by a high suspicion of lupus activity in a patient who met the definition of lupus headache (persistent nonresponsive to narcotic analgesia headache). Second, the definite diagnosis can be confirmed by an abnormal SPECT. Among diffuse and focal NPE, SPECT was useful for diffuse NPE (PLR 1.2, NLR 0.9) but not for focal NPE (PLR 1.0, NLR 1.0) (table 2).
Conclusion: The decision to perform a SPECT should be driven by a high suspicion of NPE. SPECT can be more helpful in the assessment of diffuse NPE in particular Lupus Headache and OBS/Psychosis.
To cite this abstract in AMA style:
Medina-Rosas J, Urowitz M, Su J, Gladman DD, Touma Z. Utility of the Brain Perfusion Single Photon Emission Computed Tomography in Neuropsychiatric Manifestations of Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/utility-of-the-brain-perfusion-single-photon-emission-computed-tomography-in-neuropsychiatric-manifestations-of-systemic-lupus-erythematosus/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/utility-of-the-brain-perfusion-single-photon-emission-computed-tomography-in-neuropsychiatric-manifestations-of-systemic-lupus-erythematosus/