Session Information
Date: Tuesday, November 15, 2016
Title: Muscle Biology, Myositis and Myopathies - Poster II: Clinical
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Environmental triggers such as infection are considered to be involved in pathogenesis of polymyositis (PM) and dermatomyositis (DM). This study was aimed to investigate influence of season and residential environment on development of PM/DM-associated interstitial lung disease (ILD), in association with myositis-specific autoantibodies.
Methods: This study used data recorded in a multicenter retrospective cohort of Japanese patients with PM/DM-associated ILD (JAMI cohort), which involved 44 institutions across Japan. Inclusion criteria of the JAMI cohort were adult-onset, definite or probable PM/DM including clinically amyopathic DM (CADM), ILD confirmed by imaging, and availability of serum samples at diagnosis. Demographic and clinical information was retrospectively collected by chart review, and sera were subjected to autoantibody assays; ELISA for anti-melanoma differentiation-associated gene 5 (MDA5) and RNA immunoprecipitation for anti-aminoacyl-tRNA synthetase (ARS), including Jo-1, PL-7, PL-12, EJ, OJ, and KS. Seasonality was assessed by Roger’s test in patients who developed the disease in the past 5 years. As for residential environment, we evaluated if patients’ residence at disease onset was close to the major freshwater sites. The waterfront was defined as area within 1.75 km from large river, lake, or pond calculated on the Google map.
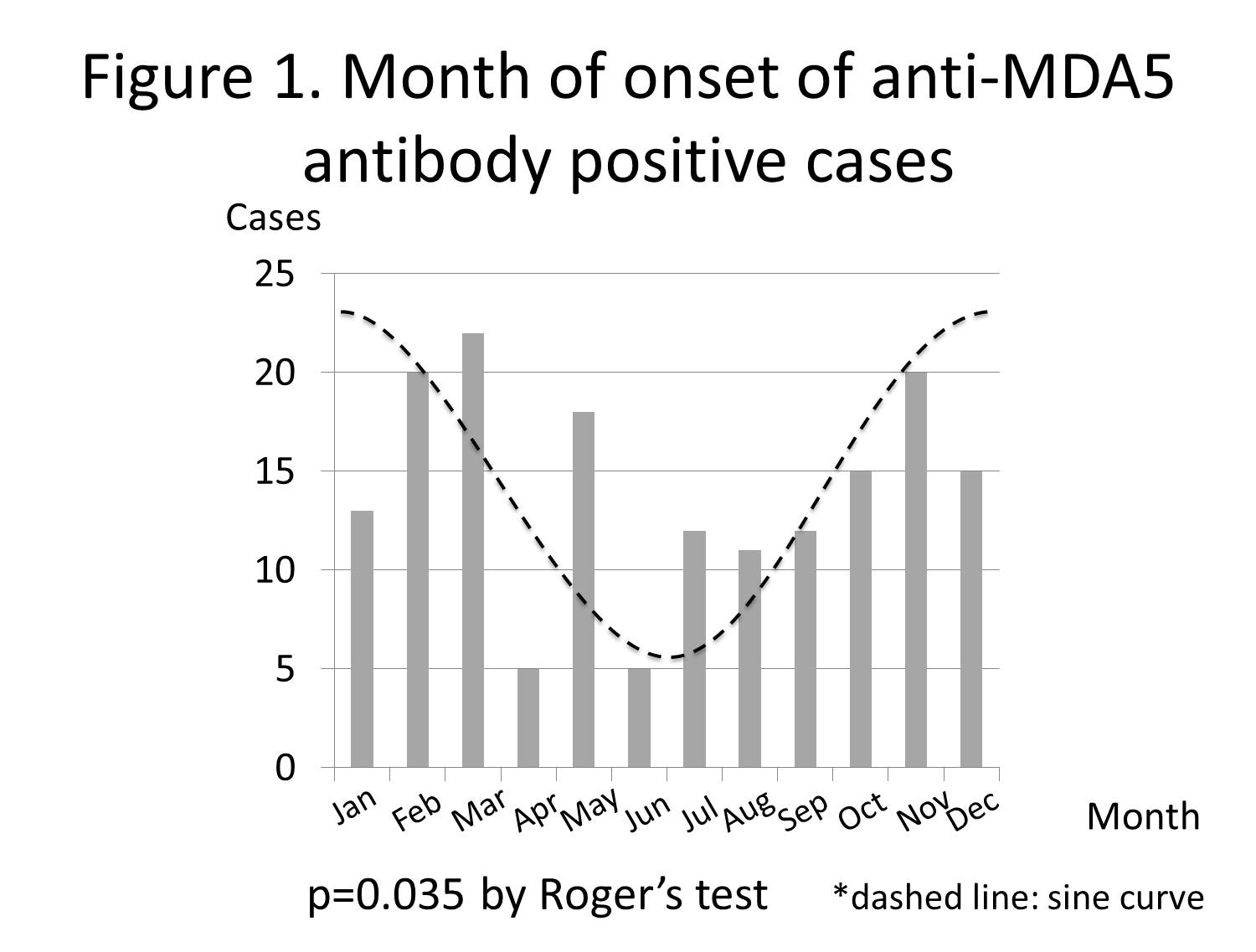
Results: Of 498 patients enrolled, anti-MDA5 and anti-ARS antibodies were detected in 212 (42%) and 165 (33%), respectively. Since one had both antibodies, 122 (24%) were regarded as the anti-MDA5/ARS-negative group. Anti-MDA5-positive patients represented a higher frequency of CADM (76% versus 24% or 30%; P <0.01 for both comparisons), and a lower cumulative survival rate at 6 months (67% versus 97% or 96%; P <0.01 for both comparisons), compared to anti-ARS-positive or anti-MDA5/ARS-negative group. Interestingly, seasonality of the disease onset was found in anti-MDA5-positive patients (P = 0.035, Figure1): more cases developed the disease in autumn/winter than in spring/summer, but not in anti-ARS-positive or anti-MDA5/ARS-negative group (P = 0.73 and 0.59, respectively). Clinical features were comparable between anti-MDA5-positive patients who developed the disease in autumn/winter and those who developed in spring/summer. The proportion of patients who resided in freshwater waterfront at disease onset was significantly higher in anti-MDA5-positive group than in anti-ARS-positive or anti-MDA5/ARS-negative group (65% versus 50% or 50%; P <0.01 for both comparisons).
Conclusion: Anti-MDA5 antibody-positive DM-associated ILD developed predominantly in autumn/winter and clustered around freshwater waterfront, suggesting roles of environmental triggers in development of the disease.
To cite this abstract in AMA style:
Nishina N, Sato S, Kawaguchi Y, Kawakami A, Tamura M, Ikeda K, Nunokawa T, Tanino Y, Asakawa K, Kaneko Y, Gono T, Masui K, Kuwana M. Influence of Season and Residential Environment on Development of Anti-Melanoma Differentiation-Associated Gene 5 Antibody-Positive Dermatomyositis with Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/influence-of-season-and-residential-environment-on-development-of-anti-melanoma-differentiation-associated-gene-5-antibody-positive-dermatomyositis-with-interstitial-lung-disease/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influence-of-season-and-residential-environment-on-development-of-anti-melanoma-differentiation-associated-gene-5-antibody-positive-dermatomyositis-with-interstitial-lung-disease/