Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Reports of associations of hypermobility and osteoarthritis (OA) vary widely. One possible cause for this lack of agreement may be different impacts of hypermobility by joint site. No prior cohort study has examined this association at the foot. This cross-sectional analysis assessed joint hypermobility with foot OA and symptoms in a large community-based cohort.
Methods: Of the 863 community-based participants with complete foot radiographs (2012-15), 848 had Beighton data (joint hypermobility; 2003-2010). Beighton criteria assessed the ability to do: passive dorsiflexion fifth finger ≥ 90 degrees, passive apposition thumb to forearm, elbow hyperextension ≥10 degrees, knee hyperextension ≥10 degrees, and palms on floor during forward trunk flexion with knees extended. One point was given for each completed maneuver (total score: 0 [unable to do any maneuver] to 9 [all maneuvers done]). Joint hypermobility was defined as Beighton score ≥4; the knee maneuver alone also was examined specifically due to the biomechanical connection of the knee and foot/ankle. Standing anteroposterior and lateral foot x-rays were read with the LaTrobe atlas to measure osteophytes (OST, 0-3) and joint space narrowing (JSN, 0-3) at five joint sites: first metatarsophalangeal, first cuneo-metatarsal, second cuneo-metatarsal, navicular-first cuneiform, and talonavicular. A joint with a score ≥2 OST or JSN was considered to have radiographic OA (rOA). Foot rOA was defined as ≥1 joint with rOA within the same foot. Foot symptoms (yes/no) was based on response to: “On most days of any one month in the last 12 months did you have pain, aching or stiffness in your left/right foot?” Separate logistic regression person-based models were used to estimate associations of foot rOA, site rOA, and symptoms with hypermobility, adjusting for covariates of age, sex, race (Caucasian vs. African American), body mass index (BMI), and history of foot injury. Pairwise interactions between hypermobility and each covariate were examined (<0.10 considered significant).
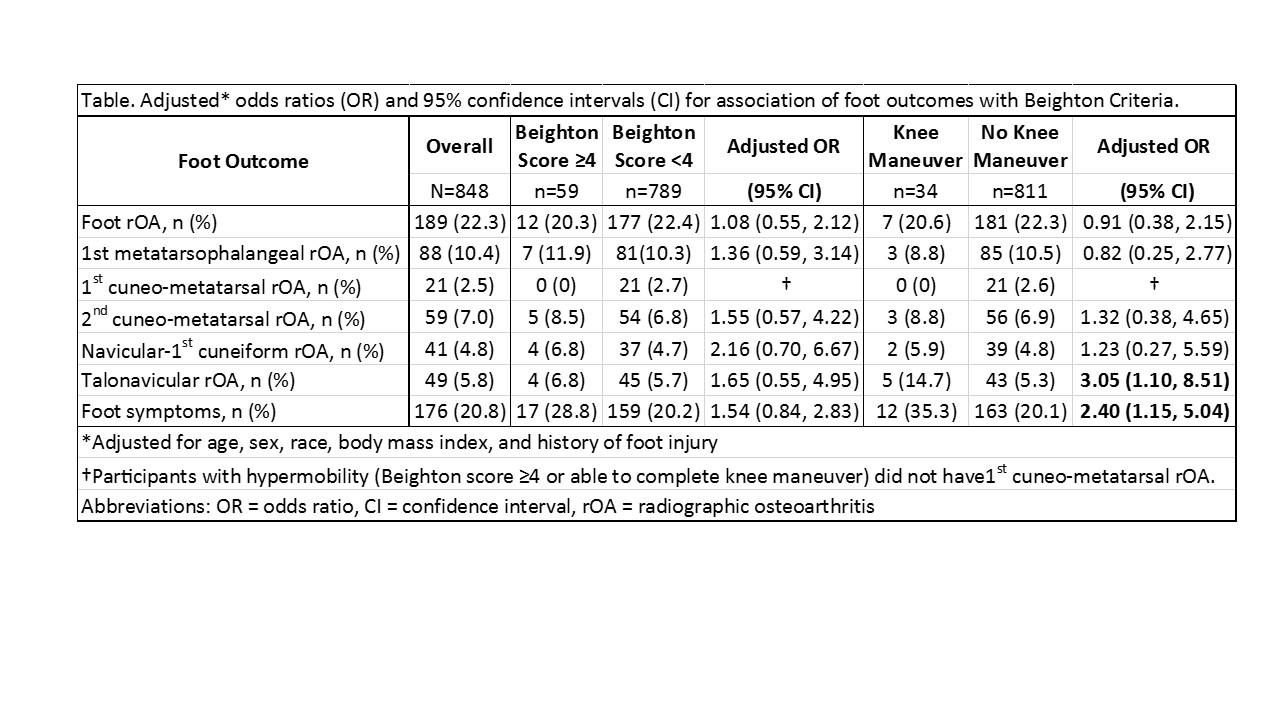
Results: This sample was 68% women and 33% African American (mean age=71 years, mean BMI=31 kg/m2). Joint hypermobility was present in 59 participants (7%); 189 (22%) participants had foot rOA, and 176 (21%) had foot symptoms. The adjusted odds of talonavicular rOA and foot symptoms were 3.0 and 2.4 times higher, respectively, among participants able vs. unable to perform the knee maneuver but based on small numbers. While no association was seen for foot rOA and hypermobility, non-significant increased estimates suggested possible relationships with specific foot joints and with foot symptoms (Table). No statistical interactions of hypermobility by covariates were observed.
Conclusion: Joint hypermobility may be related to rOA of specific foot joints and with foot symptoms. Future longitudinal studies will clarify the influence of hypermobility on the incidence and progression of foot OA and symptoms.
To cite this abstract in AMA style:
Golightly YM, Hannan MT, Nelson A, Cleveland RJ, Kraus V, Schwartz TA, Hillstrom HJ, Goode AP, Renner JB, Jordan JM. Is Joint Hypermobility Related to Foot Osteoarthritis and Symptoms? [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/is-joint-hypermobility-related-to-foot-osteoarthritis-and-symptoms/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-joint-hypermobility-related-to-foot-osteoarthritis-and-symptoms/