Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
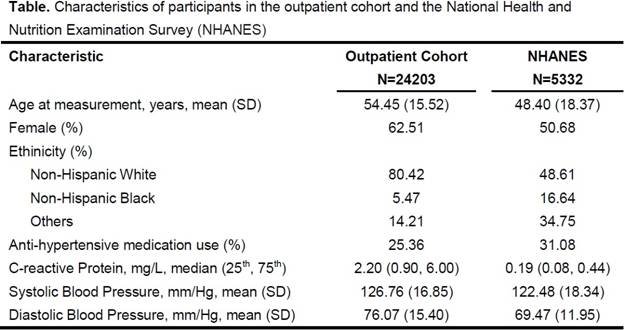
Methods : We studied all outpatients at two large tertiary care centers (Outpatient cohort), between January 1, 2009 and December 31, 2010, using data from the electronic medical records (EMR). The National Health and Nutrition Examination Survey (NHANES), a general population cohort, was studied using the same time period. Inclusion criteria for both cohorts were age>=18 years with hsCRP and BP measured on the same day. Since graphical assessment of hsCRP (common log transformed) and SBP in the outpatient cohort showed a non-linear association, we constructed a generalized additive model with penalized splines to examine the association between hsCRP and SBP. All models were adjusted for age, gender, race and use of anti-hypertensive therapy. The same method was applied to the NHANES cohort. We reviewed the medical records of 50 random patients in the highest hsCRP decile to determine the most frequent diagnosis.
Results : We studied 24,203 subjects from the outpatient cohort and 5,332 from NHANES (Table). In the outpatient cohort, we observed al non-linear relationship between hsCRP and SBP. Higher hsCRP was associated with higher SBP at hsCRP levels <7.8mg/L. At levels above 7.8 mg/L, hsCRP was inversely associated with SBP. In NHANES, we observed a linear relationship where an increase in hsCRP was associated with an increase in SBP (Figure). In the outpatient cohort, the most frequent diagnosis for patients in the highest decile hsCRP was inflammatory arthritis (50%), of which rheumatoid arthritis was the most common.
Conclusion : In a large outpatient cohort, we observed a positive linear relationship between hsCRP and SBP when hsCRP <7.8 mg/L. This relationship is consistent with previously published studies, and replicated in our NHANES analysis. However, at levels above hsCRP of 7.8 mg/L, there was an inverse relationship between hsCRP and SBP. These findings suggest the need for careful consideration of BP as a CV risk factor in patients with active inflammation.
To cite this abstract in AMA style:
Yu Z, Vanni K, Kim SC, Solomon DH, Murphy SN, Liao K. Association Between Inflammation and Systolic Blood Pressure at Normal and High C-Reactive Protein Levels [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/association-between-inflammation-and-systolic-blood-pressure-at-normal-and-high-c-reactive-protein-levels/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-inflammation-and-systolic-blood-pressure-at-normal-and-high-c-reactive-protein-levels/