Session Information
Date: Monday, November 14, 2016
Title: Rheumatoid Arthritis – Clinical Aspects II: Risk and Impact of Comorbidity
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at increased risk for infections, hospitalizations and cardiovascular (CV) events. The association of serious adverse events (SAE) with the risk of developing a stroke is unclear. We aimed to examine the cumulative incidence of strokes depending on precedent SAEs and the effect of CV treatment.
Methods: We performed a nested case-control study within the German biologics register RABBIT. Since May 2001, RA patients have been enrolled at start of a conventional synthetic (cs) or biologic (b) DMARD after ≥1 csDMARD failure. Rheumatologists report patient characteristics, comorbidities and their therapy at baseline as well as clinical status, disease activity, RA treatment and SAEs every 6 months. We considered all incident non-haemorrhagic strokes reported until October 2015 as cases. Two controls were matched to each case (Table); all but three cases could be matched. In addition, we considered all hospitalized SAEs reported before the event of stroke (index date in matched controls). We calculated the cumulative incidence of stroke depending on precedent SAEs and applied multi-state proportional hazard models.
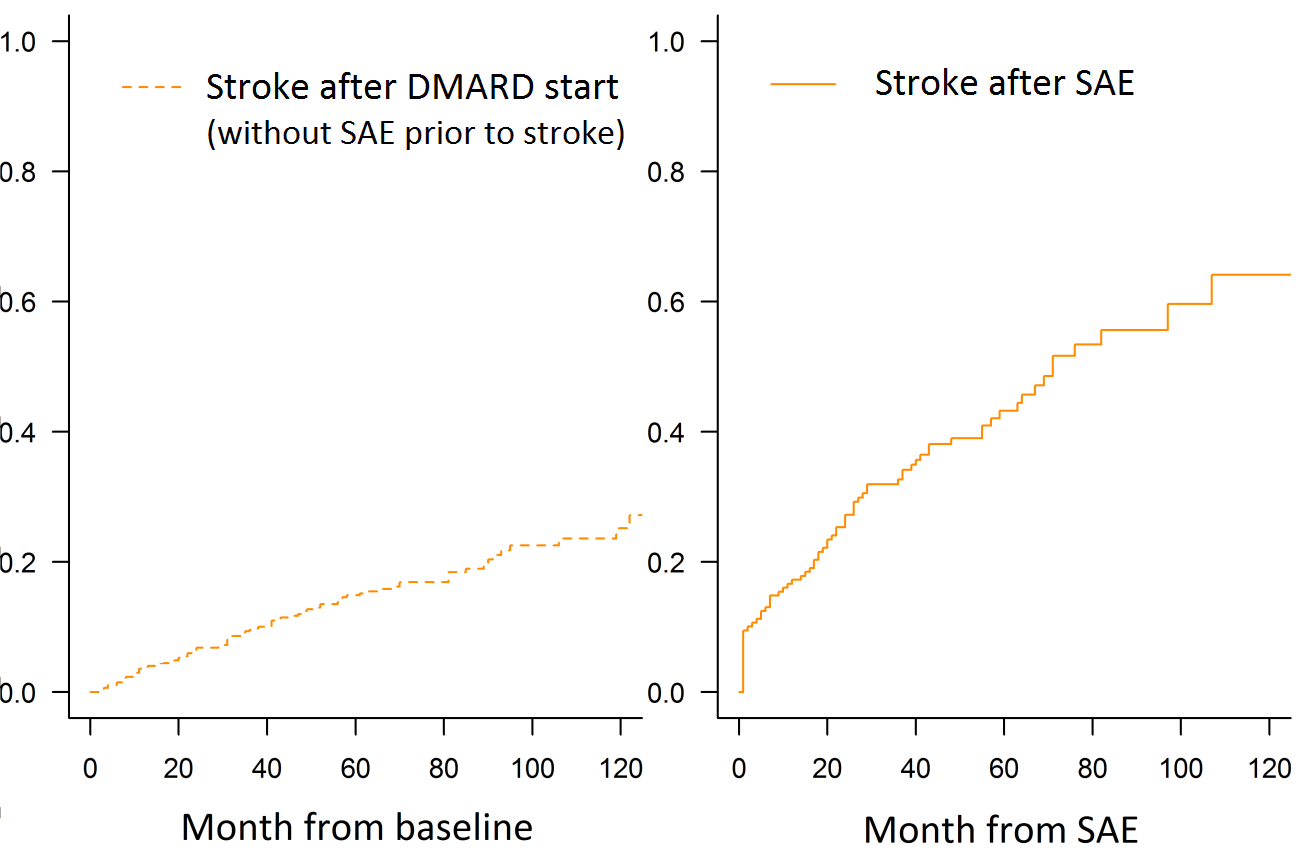
Results: Compared to the remaining cohort, cases and controls were older and had more CV risk factors. Cases and controls were similar in treatment of RA, comorbid osteoporosis, and diabetes but CV diseases were significantly less frequently treated in cases (Table). In an adjusted model, patients with treated CV diseases had a moderately elevated risk for stroke (hazard ratio (HR): 1.41 [95% CI: 0.66, 3.01]) (Ref: patients with no CV disease). In contrast, patients with untreated CV disease had a highly increased risk (HR: 3.10 [1.41, 6.79]). Treatment with TNF inhibitors or other bDMARDs was not associated with the stroke risk (HR: 0.9 [0.6, 1.4] and 0.7 [0.4, 1.2], Ref: csDMARDs). The cumulative incidence of stroke was 2.5-fold higher in patients with precedent hospitalized SAEs than in patients without (Figure). Immediately after SAEs the risk was most pronounced.
Conclusion: The risk of stroke in RA patients may be driven by precedent SAEs requiring hospitalization. In addition, untreated CV disease was a significant risk factor for a future stroke. These results strengthen the need for a better CV management in RA patients. Table: Baseline characteristics of the cohort, controls and cases.
| Parameter |
Cohort |
Controls |
Cases |
Matching |
| N |
12,598 |
316 |
158 |
2:1 |
| Age, years, mean (SD) |
55.8 (12.6)* |
62.7 (10.2) |
63.4 (10.8) |
X |
| Female gender |
9648 (76.6) |
236 (74.7) |
118 (74.7) |
X |
| Hypertension |
4638 (36.8)* |
176 (55.7) |
88 (55.7) |
X |
| Coronary heart disease |
727 (5.8) |
26 (8.2) |
13 (8.2) |
X |
| Heart failure |
283 (2.2) |
6 (1.9) |
3 (1.9) |
X |
| Diabetes |
1229 (9.8)* |
52 (16.5) |
26 (16.5) |
X |
| Smoking, never |
5381 (42.7) |
128 (40.5) |
64 (40.5) |
X |
| Enrolment prior to 2007 |
4916 (39.0)* |
172 (54.4) |
86 (54.4) |
X |
| DAS28, mean (SD) |
5.1 (1.3)* |
5.4 (1.4) |
5.5 (1.3) |
|
| CRP in mg/l, mean (SD) |
18.2 (25.9)* |
21.8 (40.1) |
23.8 (30.6) |
|
| TNFi at baseline |
6281 (49.9) |
155 (49.1) |
79 (50.0) |
|
| Other bDMARDs at baseline |
2048 (16.3) |
54 (17.1) |
31 (19.6) |
|
| Hyperlipoproteinemia |
980 (7.8)* |
37 (11.7) |
26 (16.5) |
|
| Osteoporosis |
2195 (17.4)* |
76 (24.1) |
47 (29.7) |
|
| Osteoporosis w/o treatment |
332/2195 (15.1)* |
13/76 (17.1) |
6/47 (12.8) |
|
| Diabetes w/o treatment |
239/1229 (19.4)* |
15/52 (28.8) |
3/26 (11.5) |
|
| CVD w/o treatment |
1102/5162 (21.3)* |
38/187 (20.3) |
33/100 (33.0) |
|
Values are given as numbers (%) or otherwise specified. *Statistically significant difference (p<0.05) vs. cases. Abbreviations: SD, standard deviation; w/o, without. Figure: Cumulative incidence of stroke in a case-control study: stroke without prior SAE (left), stroke after SAE (right).
To cite this abstract in AMA style:
Meißner Y, Richter A, Kekow J, Tony HP, Wilden E, Zink A, Listing J, Strangfeld A. The Risk of Stroke in Patients with Rheumatoid Arthritis and the Association with Competing Adverse Events [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/the-risk-of-stroke-in-patients-with-rheumatoid-arthritis-and-the-association-with-competing-adverse-events/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-risk-of-stroke-in-patients-with-rheumatoid-arthritis-and-the-association-with-competing-adverse-events/