Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is the leading cause of death in systemic sclerosis (SSc). Esophageal dysfunction and aspiration may play a role in SSc-ILD. We showed that esophageal dilation on high-resolution computed tomography (HRCT) scans correlated positively with radiographic ILD and negatively with forced vital capacity (FVC)1. We also showed that a widest esophageal diameter (WED) >=19mm on HRCT had the highest combined sensitivity and specificity for associated ILD2. The purpose of this retrospective, longitudinal study was to determine if a larger WED is a risk factor for SSc-ILD incidence and progression.
Methods: Subjects that fulfilled American College of Rheumatology 2013 SSc criteria with >= one HRCT and two pulmonary function tests were included. The first available HRCT was defined as the baseline exam. WED was measured. ILD was quantified by published methods3. In subjects without radiographic ILD and with baseline FVC >=70% predicted, incident restrictive lung disease was defined as new FVC <70% predicted. Change in FVC % predicted was used as a surrogate for ILD progression.
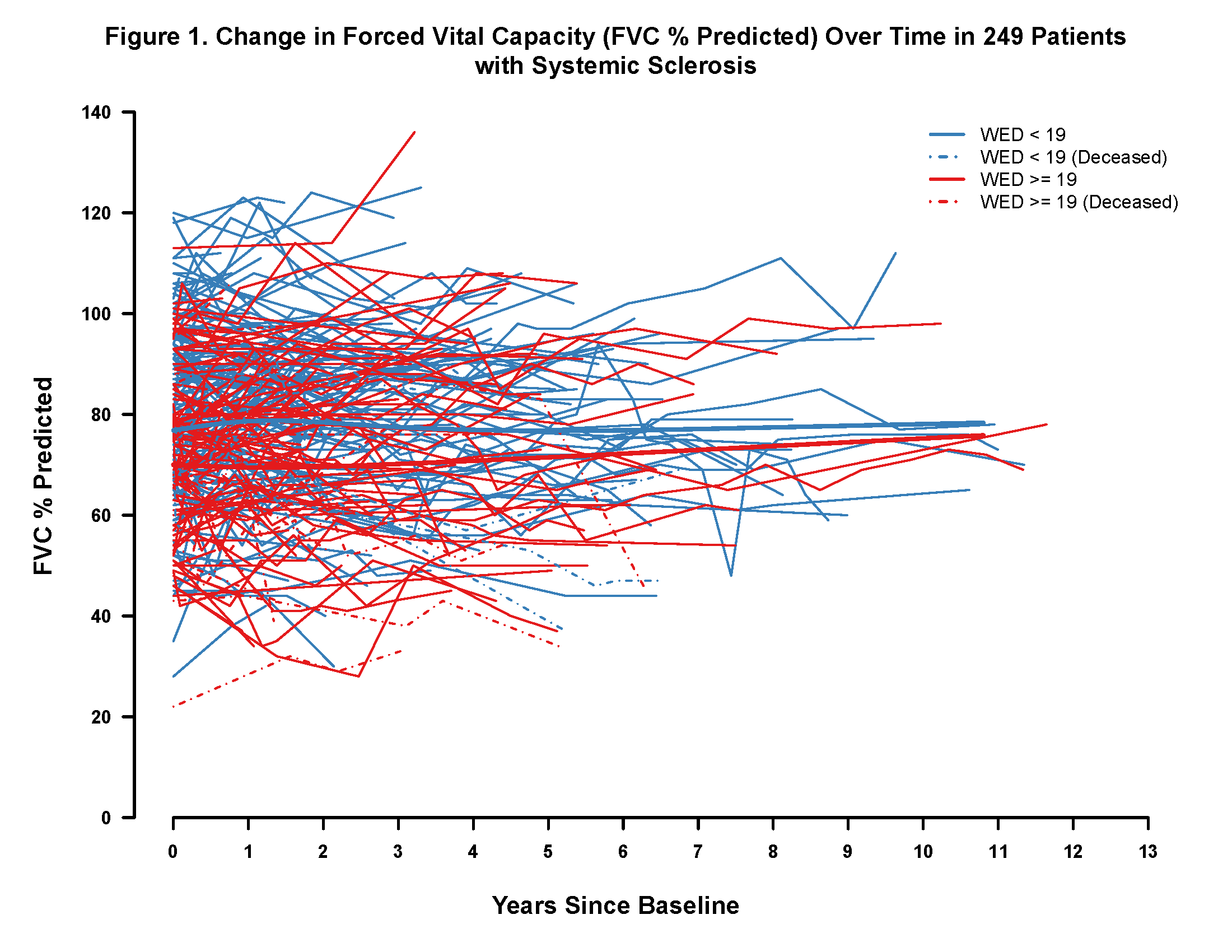
Results: In total, 249 subjects were included with a median follow up of 2.9 years (0.02-13.4y). Twenty-five subjects died. At baseline, 88 (82%) with a WED >=19mm had radiographic ILD compared with 94 (66%) with a WED <19mm (p=0.005; Table 1). Three of 55 without baseline ILD developed incident restrictive lung disease. At baseline, those with WED >=19mm had an 8.38 lower FVC % predicted than those with WED<19mm. In total, there was no clinically significant decline (i.e. >5% change) in FVC % predicted (Fig. 1). There was no significant difference in change in FVC % predicted between those with WED >=19 vs. <19mm (beta=0.2663; 95% CI -0.2256, 0.7583).
Conclusion: SSc-ILD often occurs before referral to a tertiary center. Those with a larger WED had an FVC % predicted at baseline that was clinically and statistically significantly lower than those with a smaller WED. Despite this, a larger WED at baseline was not associated with more rapid decline in FVC % predicted. References: 1. Richardson et al. Esophageal dilatation and interstitial lung disease in systemic sclerosis: a cross-sectional study. Semin Arthritis Rheum 2016 2. Hoffmann et al. Comment on: Esophageal dilatation and interstitial lung disease in systemic sclerosis: a cross-sectional study. Semin Arthritis Rheum 2016 3. Kazerooni et al. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. AJR Am J Roentgenol 1997;169:977-83 
To cite this abstract in AMA style:
Showalter K, Hoffmann A, Richardson C, Lee J, Aaby D, Agrawal R, Dematte J, Chang RW, Hinchcliff M. Esophageal Dilation and Interstitial Lung Disease Incidence and Progression in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/esophageal-dilation-and-interstitial-lung-disease-incidence-and-progression-in-systemic-sclerosis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/esophageal-dilation-and-interstitial-lung-disease-incidence-and-progression-in-systemic-sclerosis/
