Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic inflammatory arthropaties such as Rheumatoid Arthritis (RA), Psoriatic Arthritis (PsA) and Spondyloarthrities (SpA) are chronic diseases that require adequate therapies, sometimes biological drugs, to minimize inflammation and disease progression. The adherence to biologicals is supposed to be better than adherence to synthetic DMARDs, mainly methotrexate. The purpose of this study is to evaluate adherence to subcutaneous biological therapies and to assess the relationship between adherence and different demographic and clinical aspects, and its effect on clinical outcomes.
Methods: Observational retrospective study of 272 clinical records of patients with inflammatory rheumatic diseases on subcutaneous biological treatment, were reviewed. Demographic, clinical characteristics and comorbidities were compiled. Disease activity was classified as low, moderate and high based on DAS 28 in patients with peripheral arthritis and BASDAI in patients with axial SpA. Adherence was obtained for the last year from the Hospital Pharmacy registry (FARHOS). Adherence was randomly rated as good >80% of compliance, medium 60-79% and fair <59%. 11 patients not actually under biological treatment were excluded from analysis. Statistical analyses were performed using SAS for Windows statistical software, version 9.2.
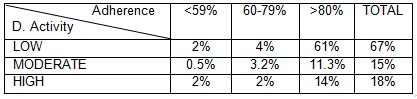
Results: From the 261 patients evaluated, 52% were female, mean aged 54 + 13.9 SD years (range 19-86). 35.6 % had RA diagnosis, 32% PsA, 29.5% axial SpA and, 6% peripheral SpA and 1% non-radiographic axial SpA. Median time of disease progression was 10.7 years. 34% presented more than two comorbidities.39% were under adalimumab, 38 % etanercept, 7.3% golimumab, 5.4% certolizumab, 4.6% tocilizumab, 2,7 % abatacept and 1% ustekinumab. 68 % were on their first biological drug, 25% on the second, and the rest had more than one biologic agent previously prescribed. 46 received concomitant synthetic DMARD. Overall adherence to biological treatment, was good, 93%, and there was no correlation between adherence and diagnose, gender, age, time of disease progression, concurrence of more than two comorbidities, cotreatment with synthetic DMARD, type of biological drug or previous treatment with other biologicals. There has been found correlation between disease activity (DAS, BASDAI) and adherence as shown in the table, P 0.0038 (Chi Square).
Conclusion: The overall adherence to subcutaneous biological therapies is very good and non-compliance has an impact in the disease activity as has been observed in this study. Therefore, it is important to check adherence when clinical response is poor to subcutaneous biological therapies and we must consider the implementation of tools to monitor adherence in order to identify non-compliant patients, quite relevant for clinical decision making.
To cite this abstract in AMA style:
Gómez-Arango C, García-Vivar ML, Alonso-Diez M, Alvarez-Lavin MM, Galindez-Agirregoikoa E, Fernández-Berrizbeitia O, Ruíz-Lucea E, María Blanco-Madrigal J, Garcia-Llorente JF, Estopiñán-Fortea L, Torre-Salaberri I, Guerrero-Basterretxea E, Calvo-Zorrilla I, Bilbao-González A, Rivera-García N. Adherence to Subcutaneous Biological Therapies Among Inflammatory Arthropaty Patients from a University Hospital [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/adherence-to-subcutaneous-biological-therapies-among-inflammatory-arthropaty-patients-from-a-university-hospital/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adherence-to-subcutaneous-biological-therapies-among-inflammatory-arthropaty-patients-from-a-university-hospital/