Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: In APS, irreversible organ damage may result of disease activity, medications, or comorbid illnesses. To assess it, different methods have been used including the SLICC index which tends to underestimate APS-related damage (Arthritis Rheum. 2011;3:Abstract). Recently, a new instrument to evaluate organ damage in APS, the Damage Index in Antiphospholipid Syndrome(DIAPS), was constructed and internally validated by adding items specific of APS that are not included in the SLICC (Lupus.2015;9:927).
Our aim was to externally validate the DIAPS in a large cohort of primary APS patients and compare its performance against the SLICC index.
Methods: A total of 77 patients with an established APS diagnosis (either primary or secondary to SLE) were recruited in our Rheumatology clinic from March to June 2016. Main demographic, clinical and laboratory data were collected and both DIAPS and SLICC indexes were simultaneously scored. In addition, anxiety (GAD-7) and depression (PHQ-9) scales were measured as surrogate of quality of life. Data were expressed as frequencies and medians (interquartile range) or means (± standard deviation) as corresponded. Differences were assessed by either Fisher’s exact or Mann-Whitney tests, while linear regressions were performed to assess linearity between DIAPS and SLICC scores. The GraphPad Prism 4.02 software was used for calculations.
Results: Out of the 77 patients included, 50 had primary APS and 27 had SLE-associated APS. Basal characteristics were similar in both groups, except for an older age (46.8±12.4 years vs 39.1±9.7 years; p=0.007) and a longer disease duration (9.6±6.4 years vs 6.0±4.8 years, p=0.01) in primary APS. Similar median DIAPS scores were found in primary APS patients as compared to secondary APS patients (2, 1 to 2.75 vs 2, 1 to 3; p=0.3); similar results were observed for the SLICC index (2, 1 to 2 vs 2, 1 to 3; p=0.3). No differences were observed for the GAD-7 (5, 2 to 6 vs 4, 1 to 5; p=0.4) and PHQ-9 (4.5, 2 to 6.25 VS 5, 2 to 6; P=0.9) indexes. No correlation was observed between the DIAPS index and either GAD-7 or PHQ-9 scores.
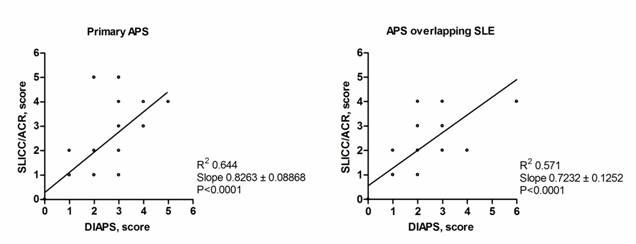
Finally, a linear association (see the Figure) between the DIAPS and the SLICC indexes was found both in primary APS patients (r2=0.64; p=0.0001) and in patients with SLE-associated APS (r2=0.57;p=0.0001).
Conclusion: Our cross-sectional study externally validates the DIAPS index as a useful instrument to evaluate cumulative organ damage in primary APS. However, it also suggests that the advantage of this current version of DIAPS over the SLICC index to assess organ damage in APS patients is marginal at best.
To cite this abstract in AMA style:
Moreno Ramirez M, Amezcua-Guerra LM, Escamilla Gomez VA, Hernandez D, Perez LF, Loaiza Felix J, Vargas Guerrero A. Performance and External Validation of the Damage Index in Antiphospholipid Syndrome in Primary and Secondary APS Patients [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/performance-and-external-validation-of-the-damage-index-in-antiphospholipid-syndrome-in-primary-and-secondary-aps-patients/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-and-external-validation-of-the-damage-index-in-antiphospholipid-syndrome-in-primary-and-secondary-aps-patients/