Session Information
Date: Sunday, November 13, 2016
Title: Health Services Research I: Workforce and Quality of Care in Rheumatology
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: We have recently found that rates of myocardial infarction (MI) are similar among individuals with SLE and those with diabetes mellitus (DM) in a nationwide cohort of Medicaid recipients. Given high cardiovascular disease (CVD) risks in both SLE and DM patients, lipid testing is widely advocated for both groups. We investigated rates of lipid testing and statin prescriptions among SLE and DM patients within Medicaid.
Methods: Within Medicaid Analytic eXtract (MAX), with billing claims from 2007-2010 for patients from the 29 most populous US states, we identified patients aged 18-65 years with prevalent SLE (
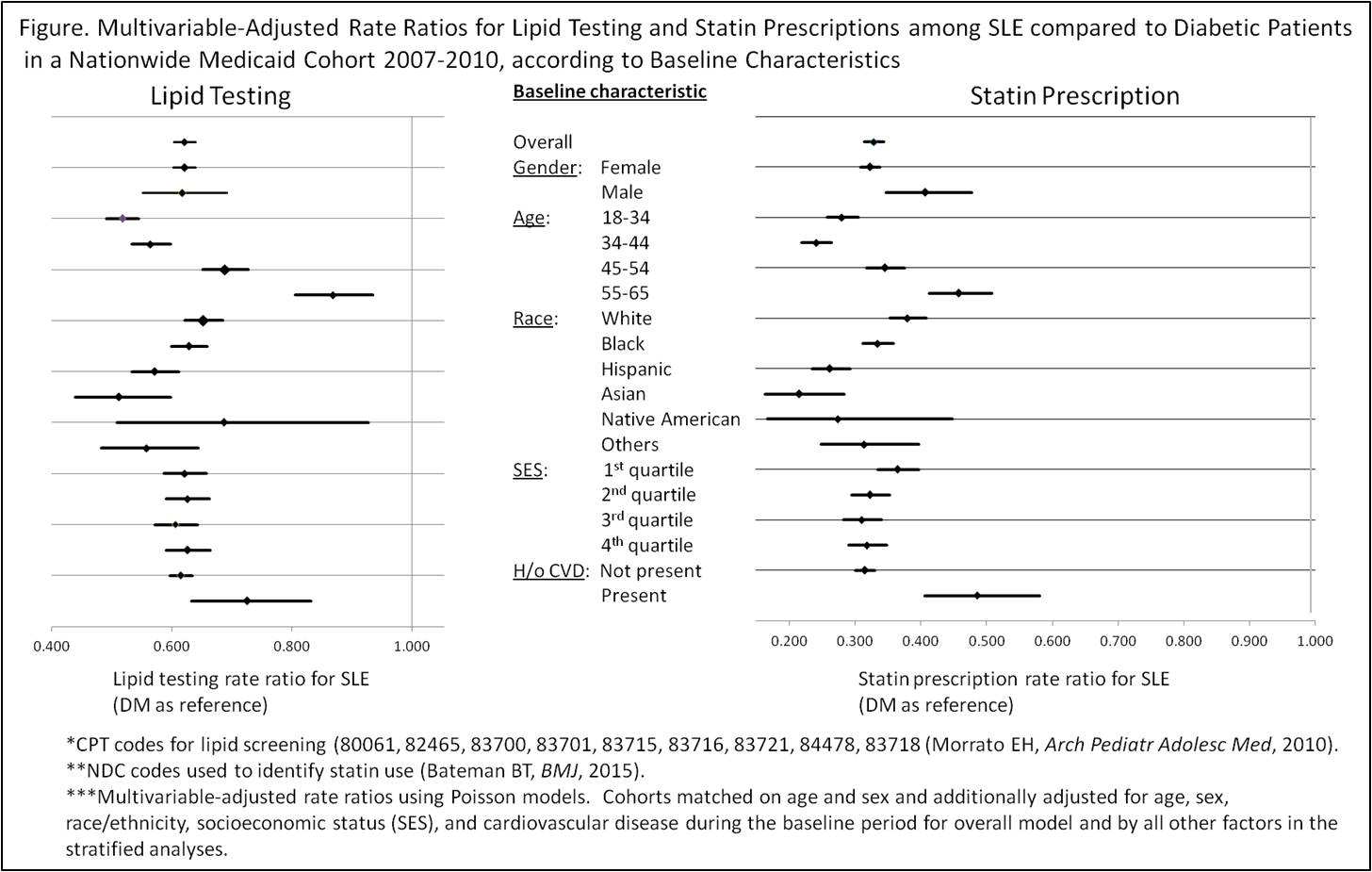
Results: 32,089 SLE patients were matched to 64,178 DM patients; 92% were female and mean age was 41.3 (
Conclusion: Rates for lipid testing and statin prescriptions increased in both SLE and DM cohorts during the study period and were highest among older patients and those with baseline CVD. Although DM and SLE confer similar risk of CVD, in this cohort, lipid testing rates were 40% lower and statin prescription rates were 70% lower in patients with SLE compared to DM.
To cite this abstract in AMA style:
Chen SK, Barbhaiya M, Fischer MA, Guan H, Lin TC, Feldman CH, Everett BM, Costenbader KH. Rates of Lipid Testing and Statin Prescriptions Among SLE and Diabetes Mellitus Patients in a Nationwide Medicaid Cohort [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/rates-of-lipid-testing-and-statin-prescriptions-among-sle-and-diabetes-mellitus-patients-in-a-nationwide-medicaid-cohort/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rates-of-lipid-testing-and-statin-prescriptions-among-sle-and-diabetes-mellitus-patients-in-a-nationwide-medicaid-cohort/