Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: We report the
results of a cluster-randomized behavioral intervention trial designed to
assess the impact of implementing a treat-to-target (T2T) approach vs usual
care (UC) in a large, US-based, observational cohort of rheumatoid arthritis
(RA) patients.
Methods: Thirty-one rheumatology practices
from the Corrona network were randomly assigned to either T2T (n=16) or UC
(n=15) between July 29, 2011 and July 30, 2013. Eligible RA patients with
moderate or high disease activity (Clinical Disease Activity Index [CDAI>10])
were followed for 12 months. In the T2T group, encounters associated with a
CDAI>10 were to result in treatment acceleration (e.g., a new initiation or
dose increase of a prescribed biologic or nonbiologic DMARD) when deemed
appropriate, with a follow-up appointment in 4 weeks. In contrast, UC patients were
seen at least every 3 months with treatment changes and follow-up visits
decided by the treating provider. Co-primary endpoints were achievement of low
disease activity (LDA; CDAI≤10) and measures of feasibility, most
importantly treatment acceleration conditional on CDAI>10. Baseline
characteristics of the T2T and UC groups were compared using standardized
differences. An intent-to-treat analysis was performed adjusting for clustering
by site and covariates associated with standardized differences >0.10.
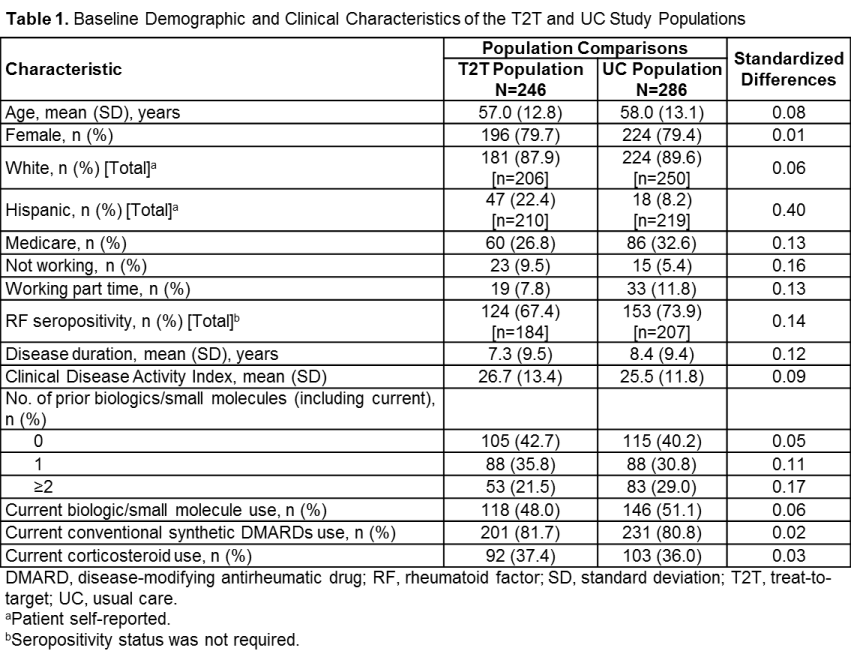
Results: There were 246 patients in the T2T
practices and 286 from UC practices enrolled. The 2 groups were similar in
terms of mean age, gender and race, but not Hispanic ethnicity (Table 1).
Patients had similar clinical features (disease duration, rheumatoid factor
seropositivity, prior medications and current medications) at baseline. During
the 12-month study period, 19.9% of the T2T group and 16.4% of the UC group
dropped out (p=0.457). Median (IQR) number of visits in the T2T group was 7.0
(5.2-9.7) compared to 4.6 (3.8-6.7) in the UC group, adjusting for clustering
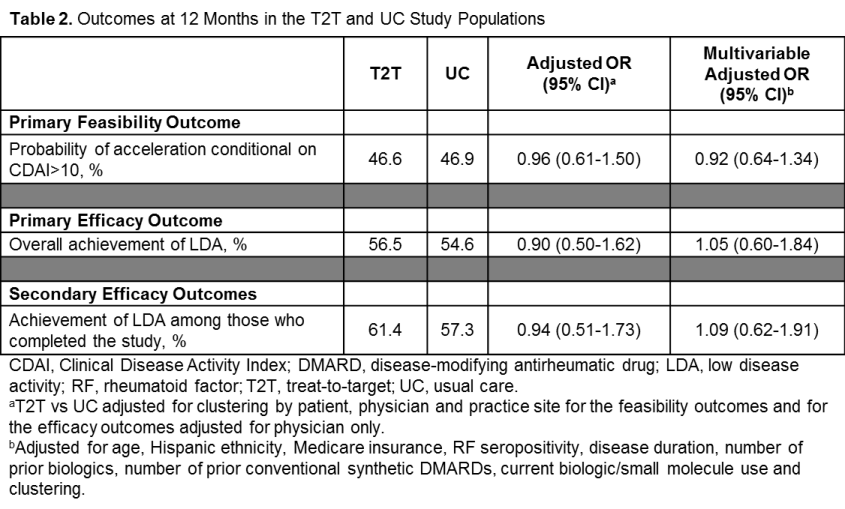
and varied person time (p<0.001). Rates of treatment acceleration and
achievement of LDA were similar in the 2 groups (Table 2). There were no
differences between the 2 arms in terms of trends in LDA over time (p=0.20).
Conclusion: This first US-based T2T
behavioral intervention in RA patients was not associated with an increased
likelihood of achievement of LDA, and acceleration occurred only ≈50% of
the time, despite providers being instructed to have more frequent visits and
accelerate therapy based upon disease activity in the T2T arm. Further analysis
is ongoing to better understand patient, provider and healthcare factors
associated with T2T implementation.
To cite this abstract in AMA style:
Harrold L, Reed GW, Harrington JT, Barr CJ, Saunders KC, Gibofsky A, Ruderman EM, Haselkorn T, Greenberg JD, John A, Kremer JM. A Cluster-Randomized Trial of a Behavioral Intervention to Incorporate a Treat-to-Target Approach in the Clinical Care of Rheumatoid Arthritis Patients in the United States [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/a-cluster-randomized-trial-of-a-behavioral-intervention-to-incorporate-a-treat-to-target-approach-in-the-clinical-care-of-rheumatoid-arthritis-patients-in-the-united-states/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-cluster-randomized-trial-of-a-behavioral-intervention-to-incorporate-a-treat-to-target-approach-in-the-clinical-care-of-rheumatoid-arthritis-patients-in-the-united-states/