Session Information
Session Type: ARHP Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose:
Osteoarthritis (OA) is
a major cause of musculoskeletal pain and disability, and is commonly reported
to impair health-related quality of life (HRQoL). We aimed to examine the
distribution of clinical OA in the hand-, knee-, and hip joints, and to investigate
whether dimensions of HRQoL differ in mono-articular and poly-articular OA.
Methods:
Postal
questionnaires regarding musculoskeletal pain, comorbidities and perceived
HRQoL, assessed by the 36-item Short Form survey (SF-36), were sent to the
general population (n=12.155, response rate 41.1%). Subsequently, those who self-reported
OA in the hand-, hip- and/or knee joint(s) (n=1045) were invited to attend a
clinical examination. 630 persons attended, of whom 547 participants free of inflammatory
rheumatic disease were analyzed. Using the
ACR-criteria for clinical OA, the participants were categorized into mono-articular
OA (MOA, i.e. OA in one single joint site) or poly-articular OA (POA, i.e. OA
in ≥ 2 joint sites) or no clinical OA (NOA). We performed
crude and adjusted linear regression analyzes with the OA categories as the
independent variable, using NOA as reference category, and the SF-36 eight
dimensions as the dependent variable.
Results:
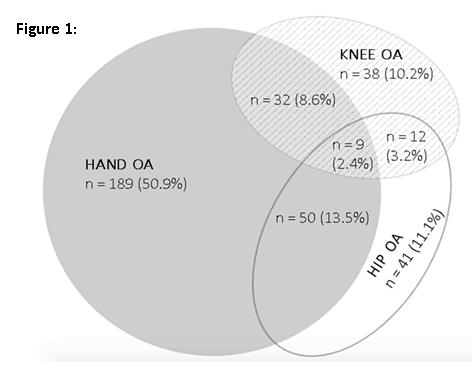
176 participants (32.2%)
were categorized into the NOA group, 268 (49%) in the MOA group and 103 (18.8%)
in the POA group (mean ± SD age 63.9 ± 8.8 years, 68% women). Clinical hand OA affected
75.5% of the OA population (Figure 1). Participants with POA had higher BMI (mean
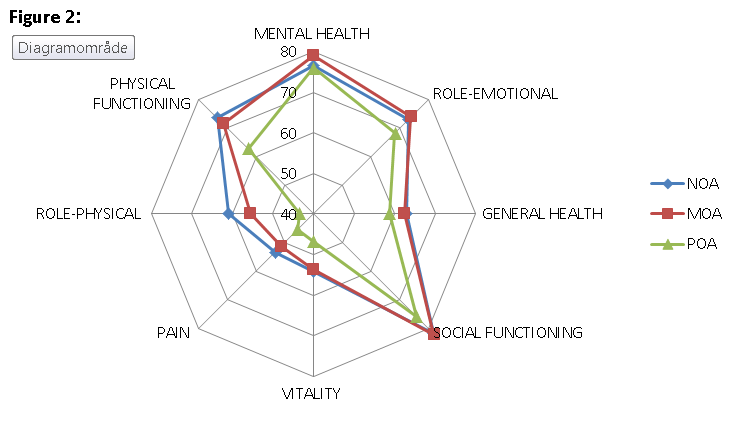
29.4 ± 4.9) compared to participants with MOA (27.6 ± 4.7) (p = 0.003). Five
out of eight SF-36 subcomponents were significantly poorer in the POA group
compared to the NOA group (Figure 2), and remained significant in analyzes adjusted
for age, gender, BMI, education and comorbidity: Social Functioning (B = -5.7,
95%CI = -11.2 to -0.1), Vitality (B = -6.7, 95% CI = -11.6 to -1.8), Pain (B = -7.5,
95% CI = -7.5 to -2.7), Physical Role (B = -15.1, 95% CI = -24.7 to -5.5) and
Physical Functioning (B = -8.8, 95% CI = -13.6 to -4.0). There were no
differences in any of the SF-36 subcomponents between the MOA and NOA groups.
Conclusion:
In a population-based cohort with
self-reported OA, approximately one third got the OA diagnosis rejected
according to the clinical ACR criteria. MOA, and specifically isolated hand OA
without affection of the knees and hips, was the most common localization of
clinical OA. POA was less prevalent, but was associated with diminished HRQoL
dimensions in terms of poorer vitality, higher pain intensity as well as impaired
physical- and social functioning compared to participants without clinical OA.
To cite this abstract in AMA style:
Økelsrud Lombnæs G, Magnusson K, Hagen KB. Distribution of Clinical Osteoarthritis and Associations to Health-Related Quality of Life in a Population-Based Osteoarthritis Cohort [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/distribution-of-clinical-osteoarthritis-and-associations-to-health-related-quality-of-life-in-a-population-based-osteoarthritis-cohort/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distribution-of-clinical-osteoarthritis-and-associations-to-health-related-quality-of-life-in-a-population-based-osteoarthritis-cohort/