Session Information
Date: Monday, November 9, 2015
Title: Spondylarthropathies and Psoriatic Arthritis - Clinical Aspects and Treatment: Clinical Aspects
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
· Background/Purpose:
Microscopic bowel inflammation
without associated gastro-intestinal symptoms is present in up to 50% of
spondyloarthritis (SpA) patients. Two types
of inflammation are distinguished based on histomorphology: an acute type
resembling infectious enterocolitis, and a chronic type, resembling early
Crohn’s disease. Microscopic bowel inflammation in SpA was shown to be associated with a more severe disease phenotype, including more
extensive bone marrow edema of the sacro-iliac joints, and an elevated risk of
progression to ankylosing spondylitis or to full-blown Crohn’s disease. Currently,
it is unknown whether microscopic bowel inflammation affects response to
therapy, particularly TNF inhibition.
Purpose: To
assess the association between the presence
of microscopic bowel inflammation, and initiation of and response to anti-TNF
therapy.
· Methods:
The Ghent Inflammatory Arthritis and spoNdylitis cohorT
(GIANT) is a prospective observational cohort study, following patients with a
new diagnosis of axial or peripheral SpA, classified according to the ASAS
criteria. Patients underwent an ileocolonoscopy at baseline to assess the
presence of microscopic bowel inflammation. For the assessment of response to
anti-TNFα treatment ASDAS scores from the moment of anti-TNF initiation
and after 3 months were compared. A clinically important improvement was
defined as an ASDAS improvement of ≧ 1.1
as recommended by ASAS.
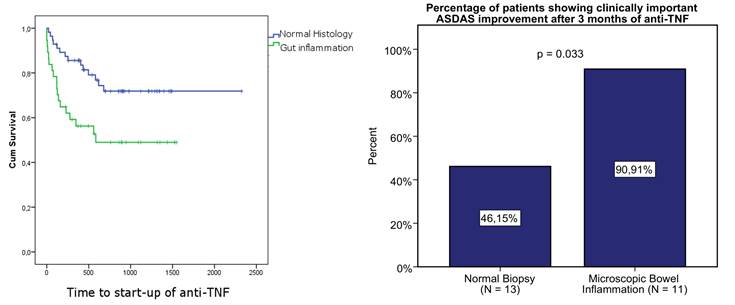
· Results:
Of the 93 patients assessed during
this study period 39,8 % were started on anti-TNF. The presence or absence of
gut inflammation was strongly linked to the rate at which anti-TNF therapy was
started (p<0.01) (Fig 1 left). Response to anti-TNF was assessed in 24 axial
spondyloarthritis patients, of which 46 % had microscopic bowel inflammation (N
acute = 4; N chronic = 7). After 3 months of anti-TNF therapy 8 (33.3%)
patients had no or slight (△<
1.1) ASDAS improvement, whereas 16 (66.7%) patients showed clinically important
improvement. Ten out of 11 (90.9%) patients with microscopic bowel inflammation
showed clinically important ASDAS improvement, whereas this was only the case
for 6/13 (46.15%) patients with normal bowel histology (p<0.05) (Fig 1
right). The association between bowel inflammation and ASDAS response remained
significant after correction for CRP using logistic regression analysis (p =
0.041; odds ratio 12.55 [1.115-141.269).
· Conclusion:
Mucosal inflammation in SpA is a risk factor for
more extended and progressive disease resulting in a higher need for TNF
inhibition. Most importantly, SpA patients with microscopic bowel inflammation
at baseline responded better to anti-TNF therapy than those with normal bowel
histology, and this association was independent of CRP. These findings
underscore the relevance of gut inflammation in the clinical course of SpA.
To cite this abstract in AMA style:
Cypers H, Varkas G, van Den Bosch F, Elewaut D. Microscopic Bowel Inflammation in Spondyloarthritis As a Baseline Predictor of Anti-TNF Response [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/microscopic-bowel-inflammation-in-spondyloarthritis-as-a-baseline-predictor-of-anti-tnf-response/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/microscopic-bowel-inflammation-in-spondyloarthritis-as-a-baseline-predictor-of-anti-tnf-response/