Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
<>Background/Purpose: Obesity and anti-citrullinated peptide
antibodies (ACPA) are risk factors for RA. We investigated whether body mass
index (BMI) and ACPA interact in determining RA risk and time to RA.
<>
<>Methods: We conducted a nested case-control study within the
Nurses’ Health Studies (NHS and NHSII). Self-reported incident RA was confirmed
by medical record review for ACR criteria. A blood sample was collected (1989-90
for NHS, 1996-99 for NHSII) prior to diagnosis among pre-RA cases and on a similar
date for controls matched on age, menopausal status and hormone use. Seven
types of novel ACPA were measured by multiplex bead-based assay (W. Robinson lab,
Stanford). For each ACPA, a value ³3 SD above the mean in controls was
considered positive. Exposures from biennial questionnaires before blood draw
included age, BMI, smoking, and alcohol intake. In the primary analysis, conditional
logistic regression models adjusting for covariates provided OR (95% CI) for developing
RA, for ACPA (³1 ACPA+), BMI, and a multiplicative interaction of ACPA and BMI (<25
vs. ³25 kg/m2). In a secondary case-only analysis, multivariable-adjusted
Cox regression models provided HR (95% CI) for time to RA. Kaplan-Meier curves
and log-rank tests compared time to RA for subgroups of pre-RA cases stratified
by ACPA and BMI.
<>
<>Results: Among 255 pre-RA cases and 778 matched controls, mean
age was 51.4 (±8.0) years and mean BMI 25.2 (±4.5) kg/m2; 98% were
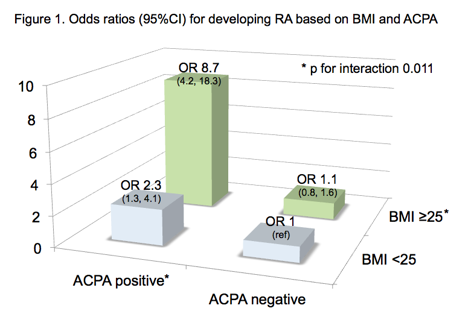
White and 11.4% were ACPA+. In multivariable conditional logistic regression,
there was a significant interaction between ACPA+ and BMI ³25 for RA risk
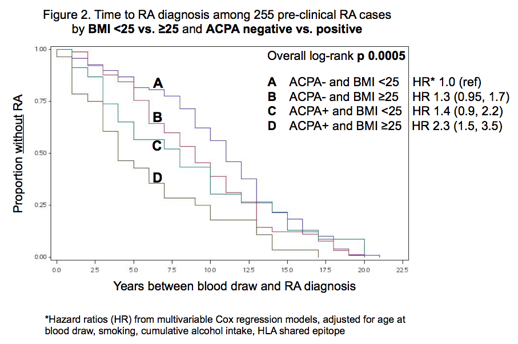
(p 0.011) (Fig. 1) Among pre-RA cases, mean time to RA was 8.9 (± 5.3) years after
blood draw. Time to RA was shortest among those with BMI ³25 and ACPA+ (5.3 ±
4.8 years) and longest in those with BMI<25 and ACPA- (10.5 ± 5.0 years) (log
rank p 0.0002). In multivariable Cox models, women with BMI ³25 and ACPA+ had
the highest risk for RA (HR 2.3, 95%CI 1.5, 3.5) (Fig. 2).
<>
<>Conclusion: Among women who later developed RA and matched
controls, elevated BMI and ACPA+ interacted to increase RA risk, suggesting
that these factors are synergistic. Time to RA was shortest in pre-RA cases with
both elevated BMI and ACPA+. Obesity may accelerate onset of RA in particular
among those who are already ACPA+. The biological mechanism behind our findings
warrants further investigation.
antibodies (ACPA) are risk factors for RA. We investigated whether body mass
index (BMI) and ACPA interact in determining RA risk and time to RA.
<>
<>Methods: We conducted a nested case-control study within the
Nurses’ Health Studies (NHS and NHSII). Self-reported incident RA was confirmed
by medical record review for ACR criteria. A blood sample was collected (1989-90
for NHS, 1996-99 for NHSII) prior to diagnosis among pre-RA cases and on a similar
date for controls matched on age, menopausal status and hormone use. Seven
types of novel ACPA were measured by multiplex bead-based assay (W. Robinson lab,
Stanford). For each ACPA, a value ³3 SD above the mean in controls was
considered positive. Exposures from biennial questionnaires before blood draw
included age, BMI, smoking, and alcohol intake. In the primary analysis, conditional
logistic regression models adjusting for covariates provided OR (95% CI) for developing
RA, for ACPA (³1 ACPA+), BMI, and a multiplicative interaction of ACPA and BMI (<25
vs. ³25 kg/m2). In a secondary case-only analysis, multivariable-adjusted
Cox regression models provided HR (95% CI) for time to RA. Kaplan-Meier curves
and log-rank tests compared time to RA for subgroups of pre-RA cases stratified
by ACPA and BMI.
<>
<>Results: Among 255 pre-RA cases and 778 matched controls, mean
age was 51.4 (±8.0) years and mean BMI 25.2 (±4.5) kg/m2; 98% were
White and 11.4% were ACPA+. In multivariable conditional logistic regression,
there was a significant interaction between ACPA+ and BMI ³25 for RA risk
(p 0.011) (Fig. 1) Among pre-RA cases, mean time to RA was 8.9 (± 5.3) years after
blood draw. Time to RA was shortest among those with BMI ³25 and ACPA+ (5.3 ±
4.8 years) and longest in those with BMI<25 and ACPA- (10.5 ± 5.0 years) (log
rank p 0.0002). In multivariable Cox models, women with BMI ³25 and ACPA+ had
the highest risk for RA (HR 2.3, 95%CI 1.5, 3.5) (Fig. 2).
<>
<>Conclusion: Among women who later developed RA and matched
controls, elevated BMI and ACPA+ interacted to increase RA risk, suggesting
that these factors are synergistic. Time to RA was shortest in pre-RA cases with
both elevated BMI and ACPA+. Obesity may accelerate onset of RA in particular
among those who are already ACPA+. The biological mechanism behind our findings
warrants further investigation.
Disclosure: S. K. Tedeschi, None; J. Cui, None; E. V. Arkema, None; J. A. Sparks, None; E. W. Karlson, None; K. H. Costenbader, Arthritis Care and Research, 5,International Journal of Clinical Practice, 5.
To cite this abstract in AMA style:
Tedeschi SK, Cui J, Arkema EV, Sparks JA, Karlson EW, Costenbader KH. Elevated BMI and ACPA Together Increase RA Risk and Independently Accelerate Time to RA [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/elevated-bmi-and-acpa-together-increase-ra-risk-and-independently-accelerate-time-to-ra/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/elevated-bmi-and-acpa-together-increase-ra-risk-and-independently-accelerate-time-to-ra/