Session Information
Date: Monday, November 9, 2015
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment Poster Session II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
SLE
patients develop non-deforming non-erosive (NDNE) arthritis
in 70-80%, but 5-15% of cases progresses into Jaccoud’s
arthropathy (JA) a non-erosive deforming arthritis. This
study was aimed to investigate risk factors for development of JA in SLE
patients with a focus on the progression and predictive values of synovitis,
tenosynovitis and erosions detected by high-resolution ultrasound (US).
Methods:
Ninety-four
consecutive patients diagnosed with SLE and NDNE musculoskeletal involvement
were recruited in a 5-year prospective follow-up study. Sixty healthy subject
served as controls.
Every
6 months, or more frequently according to clinical needs, each patients
underwent physical examination and a large panel of laboratory investigations.
The occurrence of musculoskeletal flares was evaluated using the musculoskeletal
item of BILAG2004 index. X-ray and US examination were performed at baseline
and at the end of study. Patient reported outcomes (PROs) by means of SF36v2,
HAQ and VAS-Pain were assessed.
Clinical,
serological and US findings were used as covariates to identify risk factors
for development of hand deformities (according to Spronk
PE, et al. Ann Rheum Dis 1992;51:358-61).
Stepwise Cox proportional hazard and logistic regression models were fitted
with covariates with p<0.1 to predict outcomes; p<0.05 was considered
significant. Odds ratio (OR) with 95% confidence interval (95% CI) was
calculated.
Results:
Eighty
patients (mean age 45.5±13.2 years; disease duration 10.7±7.1 years) completed the
5-year follow-up. Hand deformities developed in 5 (6.2%) patients with a JA
estimated incidence rate of 1.25 per 100
patient-year. Longer disease duration (p=0.010; OR 1.3 95%CI 1.1-1.5) and MS
flares during follow-up (p=0.017 ; OR 7.0 95%CI 1.4-35.5) independently conferred
an increased risk for development of JA.
Over 860 clinical assessments, 13 musculoskeletal flares (3 “A” severe and 10
“B” moderate) in 10 (12.5%) patients were recorded. US evidence of synovial
proliferation with power-Doppler signal in joints or tendons (p=0.005;
RR 6.7 95%CI 1.8 – 22.6) was the only
independent risk factor for musculoskeletal flare. New US erosions were
detected in 13 (19.7%) patients but none of them had erosions on X-ray. Active
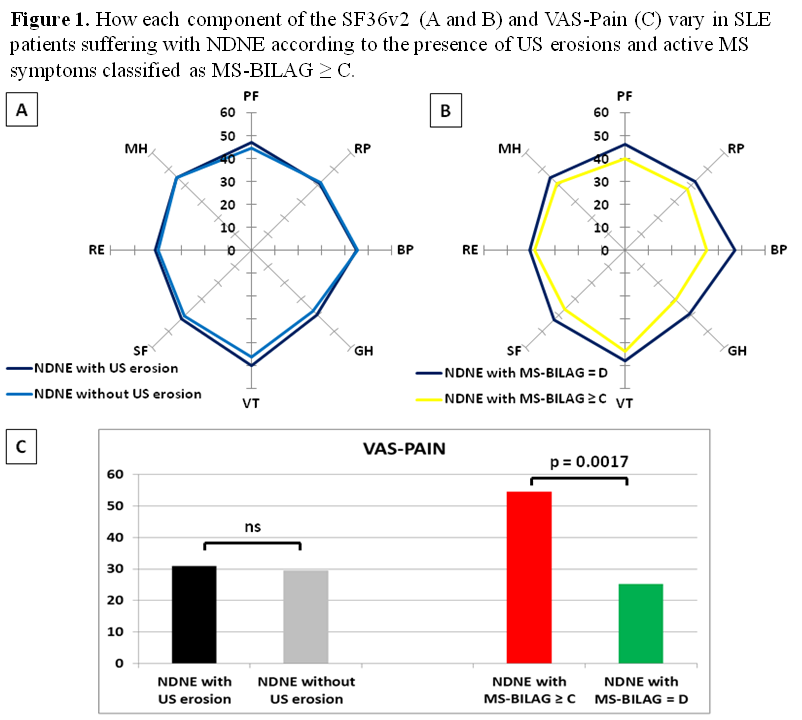
musculoskeletal involvement was responsible of worse PROs than detection of US
erosions (Figure 1).
Conclusion:
Development
of JA was more likely in patients with
musculoskeletal flares and longer disease duration. US abnormalities identify a
subset of SLE patients with more aggressive musculoskeletal involvement, higher
risk for flares and, therefore, at risk for development of JA and deterioration
of PROs.
To cite this abstract in AMA style:
Piga M, Gabba A, Congia M, Figus F, Floris A, Cauli A, Mathieu A. Predictability of Musculoskeletal Flares and Hand Deformities in Systemic Lupus Erythematosus By High Resolution Ultrasound : 5-Year Clinical and Imaging Prospective Follow-up Study [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/predictability-of-musculoskeletal-flares-and-hand-deformities-in-systemic-lupus-erythematosus-by-high-resolution-ultrasound-5-year-clinical-and-imaging-prospective-follow-up-study/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictability-of-musculoskeletal-flares-and-hand-deformities-in-systemic-lupus-erythematosus-by-high-resolution-ultrasound-5-year-clinical-and-imaging-prospective-follow-up-study/