Session Information
Date: Monday, November 9, 2015
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment Poster Session II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Women with SLE have an increased
incidence of premature cardiovascular disease (CVD). Depression is also common
among SLE patients. A relationship between depression and increased
inflammation leading to CVD has been proposed. The aim of this study was to
evaluate the relationship between depression and the progression of subclinical
CVD in women with SLE.
Methods: In a prospective case-control study, the Study of Lupus Vascular and
Bone Long-term Endpoints (SOLVABLE), there were 185 women with SLE meeting ACR
revised classification criteria and 186 controls. Participants were evaluated
at baseline and 5 years, including demographic data, laboratory studies, CVD
risk factors, depression screening with the Center for Epidemiologic Studies
Depression Scale (CES-D) questionnaire, ultrasound evaluations of carotid
artery intima-media thickness (IMT) and carotid
plaque, and assessment of SLE disease activity and damage for the SLE cases.
Depression was defined as CES-D score > or = 16. Plaque progression was
defined by an increase in number of plaques over 5 years. IMT progression was
defined as increase in IMT over 5 years.
HTN was defined as systolic blood pressure (BP) >140mmHg, diastolic
BP >90mmHg, or taking anti-hypertensive medication. Descriptive statistics
were calculated for baseline variables. Logistic regression was used to
evaluate the association between baseline depression and the progression of
carotid plaque. Linear regression was used for baseline depression and
progression of IMT.
Results: A total of 149 participants with SLE and 126 controls completed
follow-up over 5 years. The SLE group was younger (48.6 years vs. 52.2,
p=0.003) and had more hypertension (HTN) (57.7% vs. 31.8%, p<.0001), diabetes (9.4% vs. 0.8%, p=0.01) and aspirin use
(20.8% vs. 7.1%, p=0.001). There were no significant differences between the
groups regarding race/ethnicity, BMI, total cholesterol/high density
lipoprotein (HDL) ratio, or statin use. The SLE group had a higher rate of
depression, 40% compared with 15% in the control group (p <0.001). The
average SLE disease duration was 12 years (SD 8.6 years), and baseline SLEDAI
2000 and ACR/SLICC scores were 4.0 (SD 3.6) and 1.6 (SD 1.8), respectively. In
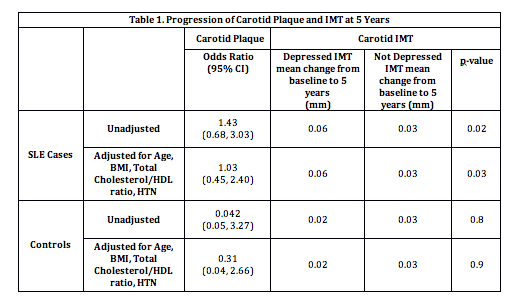
Table 1, in both the unadjusted and adjusted models, the presence of baseline
depression correlated with increased progression of IMT in the SLE group, but
not in the control group. There was no association between depression and
carotid plaque in either group.
Conclusion: Women with SLE have higher rates of depression than healthy peers.
SLE patients with depression have an increased risk of developing subclinical
CVD, as measured by IMT, a more sensitive measure of atheroma burden, but not by carotid plaque. The data suggest that
depression, a potentially modifiable risk factor, may contribute to the
increased risk of subclinical CVD in women with SLE.
To cite this abstract in AMA style:
Jorge A, Lertratanakul A, Lee J, Pearce W, McPherson D, Thompson T, Barinas-Mitchell E, Ramsey-Goldman R. Depression and Progression of Subclinical Cardiovascular Disease in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/depression-and-progression-of-subclinical-cardiovascular-disease-in-systemic-lupus-erythematosus/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/depression-and-progression-of-subclinical-cardiovascular-disease-in-systemic-lupus-erythematosus/