Session Information
Date: Monday, November 9, 2015
Title: Quality Measures and Quality of Care Poster Session (ARHP): Clinical Practice/Patient Care
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite routine blood pressure (BP) measurement by
clinic staff, we reported that rheumatologists discussed elevated BPs in
<1/3 of visits leading to missed opportunities for cardiovascular disease prevention.
Staff-driven hypertension protocols in primary care reduce such variation by
empowering clinic staff. Our objective was to engage clinic staff in work
system redesign to develop and implement a blood pressure protocol adapted to
specialty care. We report results of this process under the five work system
domains: people, tools, organization, environment, and tasks.
Methods: Our multidisciplinary team engaged clinic
staff (medical assistants (MA), nurses (RN), and schedulers) in work system redesign.
Three discipline-specific one hour focus groups appraised pre-visit rooming and
check-out workflows, our proposed protocol, and electronic health record (EHR)
tools. Staff participated in a 45 min group session on BP, and one-on-one 15
min EHR training sessions. We audited fidelity through EHR data and provided
monthly individual audit feedback. These brief sessions focused on goal-setting
and staff-driven problem-solving. Three later focus groups offered us
evaluative feedback and suggestions for improvements. We also administered a
retrospective anonymous 15 item staff questionnaire after pilot testing.
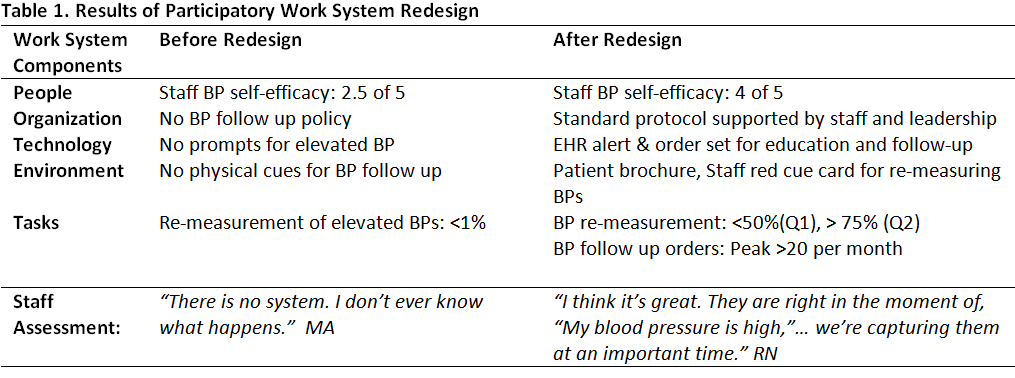
Results: Over 90% (9 MAs, 5 RNs, 4 schedulers) of
staff participated in focus groups. Content analysis of the focus groups
informed the development and implementation of work system redesign
interventions (Table 1). The work system redesign included training (people),
protocol and workflows adapted to specialty care (organization, tasks), a
customized EHR alert for elevated BP and EHR follow-up order set (technology),
and supportive physical cues like a desktop patient brochure linking
rheumatologic conditions and heart risk (environment). Four monthly audit
feedback sessions with 10 regular MAs or RNs identified barriers and solutions.
All staff met progressively higher goals and achievement. In evaluative
focus groups staff voiced satisfaction and suggested pragmatic changes
including BP re-measurement red cue cards and EHR alert revisions.
Questionnaires showed improved BP self-efficacy post intervention.
Conclusion: We engaged rheumatology clinic staff in
participatory work system redesign to improve follow up for patients with
elevated blood pressure. The collaborative redesign process resulted in
successful modification and implementation of a blood pressure protocol for
specialty care. Results suggest sound intervention feasibility including
improved staff self-efficacy and demonstrate good intervention fidelity
including improved BP re-measurement and follow up orders over time.
To cite this abstract in AMA style:
Ramly E, Lauver D, Bartels CM. Engaging Clinic Staff in Work System Redesign to Adapt a Hypertension Protocol for Rheumatology [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/engaging-clinic-staff-in-work-system-redesign-to-adapt-a-hypertension-protocol-for-rheumatology/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/engaging-clinic-staff-in-work-system-redesign-to-adapt-a-hypertension-protocol-for-rheumatology/