Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
We have previously described (Nature Medicine, PNAS, A&R, Nature
Rheum, Lancet)
how oral treatment with the pro-inflammatory, heat shock protein-derived dnaJP1
peptide induces detectable clinical amelioration in Phase I and IIa clinical
studies in rheumatoid arthritis. In previous work, we have also identified T
effector (Teff) immune deviation and an increase in
PD-1 Treg subsets as some of the immune mechanisms leading to clinical
improvement. Clinical and immunological data also emphasized a synergistic
effect with hydroxychloroquine (HCQ). Our previous studies, however, did not capture, yet, the complexity of the dynamic interactions among subsets of
immune cells. Here, we apply a novel approach aiming at addressing this unmet
need.
Methods:
Patient selection, randomization treatment and assessment
of clinical outcomes were previously described (Koffeman, et al 2009, Arthritis &
Rheumatism). Antibody panels were designed, based on previous specific experience and data, to encompass the
major subsets of immune cells and employed to study by flow cytometry PBMCs
from two treatment cohorts: (a) dnaJP1-HCQ responders (n=6) (b) Placebo HCQ Non
Responders (n=10)
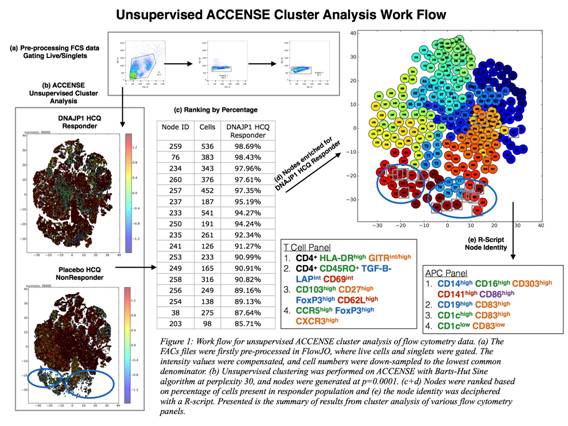
We have substantially modified and adapted for use
in translational research the clustering software ACCENSE (Shekhar, et al,
2014, PNAS). The work flow is presented in Fig. 1,
and FD is defined as fold difference percentage of responders over non
responders cells.
Results:
T cell subsets which were significantly more represented in
dnaJP1 responders were antigen experienced, activated T cells which displayed tolerogenic/regulatory characteristics (CD4+CD45RO+TGF-BintCD69int , FD= 17) and (CD4+HLA-DRhiGITRint/high, FD = 27). Intriguingly we also detected FoxP3hi T cells which may represent regulatory
subsets transiting between inflammatory (CCR5hiCXCR3hi, FD = 9) and
mucosal (CD103hiCD27hiCD62Lhi, FD = 7) compartments.
Analysis of the antigen presentation cells (APCs)
compartment revealed two functionally distinct subsets which are significantly elevated in dnaJP1 clinical
responders, both subsets probably the outcome of
cross talk between tolerized/regulatory T cells and APC: (a) CD14+CD16+CD303hiCD141hi (FD = 10) monocytes that exhibit CD86hi expression, which has been described to
relate to and augment Treg function, (b) APCs which manifest a mature phenotype (CD83+), subdivided into 3 lineages (i) CD19hi B cells (FD = 9), (ii) dendritic cells CD1chi (FD = 72) and (iii) CD1clo (FD = 19).
Conclusion:
A holistic approach to the immunome confirmed the
specificity and complexity of the immune tolerization mechanism, which relies on
the interplay between effector and regulatory T cells and APC. This approach
has a dual translational value, as it provides mechanistic knowledge and also
potential biomarkers directly related to the therapeutic intervention.
To cite this abstract in AMA style:
Leong JY, Ong R Jr., Li J, Broek TVD, Spreafico R, Rossetti M, Albani S. Deciphering the Immunome of Clinically Effective Immune Tolerization in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/deciphering-the-immunome-of-clinically-effective-immune-tolerization-in-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/deciphering-the-immunome-of-clinically-effective-immune-tolerization-in-rheumatoid-arthritis/