Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Because the clinical manifestations of NPSLE are diverse, multifaceted approaches are necessary to evaluate the disease activity and therapeutic responses. We investigated contribution of various CNS examinations to clinical assessment in each subtype of NPSLE.
Methods: We retrospectively analyzed clinical features and the findings of CSF, EEG, CNS imaging modalities including MRI and SPECT in 41 patients (6 male, 35 female) who met ACR 1997 SLE classification criteria with neuropsychiatric symptoms from 2000 to 2011. The patients were categorized into 3 groups according to ACR-defined NPSLE syndromes at 1999; Patients with neurological symptoms (Group N), those with psychiatric symptoms (Group P), and those with the both (Group N+P).
Results: Median age at onset of SLE was 25 years old (range 5-63). About a half of the patients developed neuropsychiatric symptoms within a year from SLE onset. Based on the clinical symptoms such as cognitive dysfunction (37%), acute confusional state (32%), seizure (29%), headache (22%), aseptic meningitis (20%), and cerebrovascular disease (15%), the patients were classified into Group N (16 patients, 39%), Group P (13 patients, 32%), and Group N+P (12 patients, 29%). Pleocytosis and increased protein in CSF were the most frequently found in Group N, whereas increased protein with high IgG index was also observed in a part of patients in Group P. EEG abnormality, especially emergence of slow waves, was more prevalent in group P and N+P than group N. MRI showed any abnormalities in 85 %. Diffuse white matter (WM) high intensity signals in Group N, and cerebral parenchymal atrophy and focal WM high intensity signals in group P and N+P were common. SPECT revealed the hypoperfusion, particularly in the frontal and parietal lobes in all patients but one, even in those having normal MRI. Most patients received potent immunosuppressive therapies including steroid pulse and IVCY, leading to clinical improvement in 69% of Group N but 37.5% of Group P and N+P, irrespective of pre-therapeutic clinical parameters. In 19 patients having follow-up examinations of SPECT, brain perfusion was restored with clinical amelioration responding the therapy in 4 out of 5 patients of Group N. In contrast, hypoperfusion was unchanged or decreased in about 75%, 50% of Group P, N+P, respectively. In the two groups, there was a discrepancy between SPECT findings and clinical course in 5 of 14 patients.
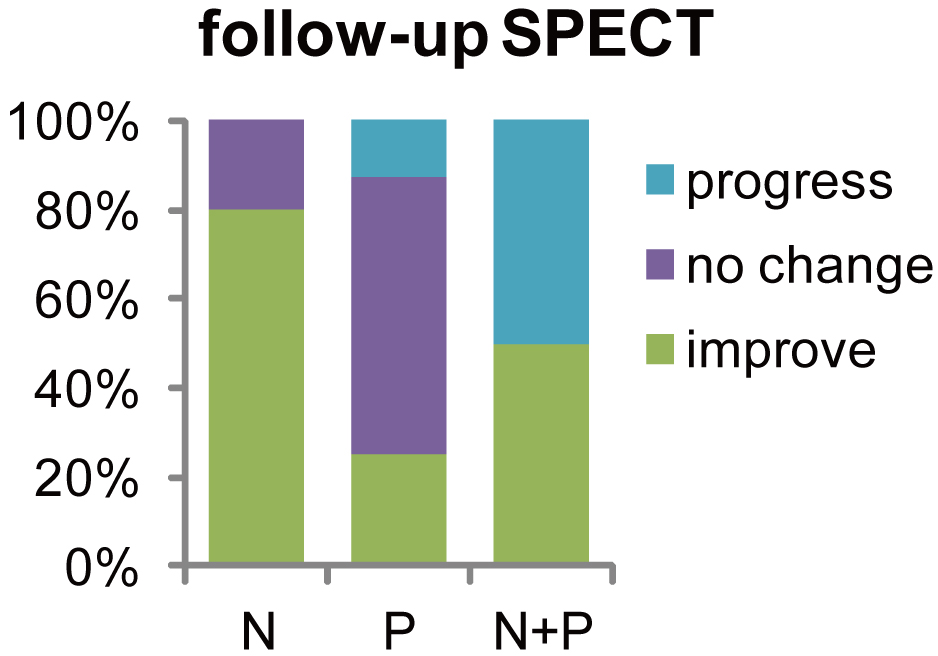 |
Conclusion: Cerebral hypoperfusion in SPECT was associated with NP lesions in SLE and the findings were closely correlated with disease activity especially in neurological deficits rather than psychiatric symptoms.
Disclosure:
M. Hama,
None;
M. Takeno,
None;
A. Ihata,
None;
D. Kishimoto,
None;
R. Watanabe,
None;
T. Uehara,
None;
R. Yoshimi,
None;
Y. Asami,
None;
A. Ueda,
None;
Y. Ishigatsubo,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/single-photon-emission-computed-tomography-contributes-to-clinical-assessments-in-neuropsychiatric-systemic-lupus-erythematosus-patients/
