Session Information
Date: Wednesday, November 16, 2016
Title: Osteoarthritis – Clinical Aspect II: Treatment and Imaging
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: In the treatment of meniscal damage in the setting of mild to moderate osteoarthritis (OA), several randomized trials found that both arthroscopic partial meniscectomy (APM) and physical therapy (PT) led to substantial pain relief. Whether certain subgroups of patients have worse outcomes with APM vs. PT is unknown. We hypothesize that increased baseline cartilage damage and presence of bone marrow lesions (BML) on magnetic resonance imaging (MRI) modifies the efficacy of APM compared to PT.
Methods: We used the data from the Meniscal Tear in Osteoarthritis Research (MeTeOR) Trial of APM vs. PT. Subjects were ≥45 years old and had meniscal damage on MRI, evidence of OA changes on imaging, and knee symptoms. Patients who were randomized to APM generally had surgery within three weeks after randomization. Patients who crossed-over between treatment groups were excluded from this analysis. MRIs were read using the MRI OA Knee Score (MOAKS). All 15 subregions were analyzed. Maximum, cartilage damage in any subregion (% of loss that is full thickness) was dichotomized at <10% vs. ≥10% and maximum BML in any subregion (% of subregion occupied) at none vs. any. The outcome was change from baseline to 6 months in the Knee Injury and Osteoarthritis Outcome Pain Score (KOOS, scored 0-100, 100 worst). We investigated the interaction between the imaging variables (cartilage damage, BML), treatment type (APM, PT) and change in KOOS Pain. We then calculated the difference in mean change between those receiving APM and PT for each imaging category.
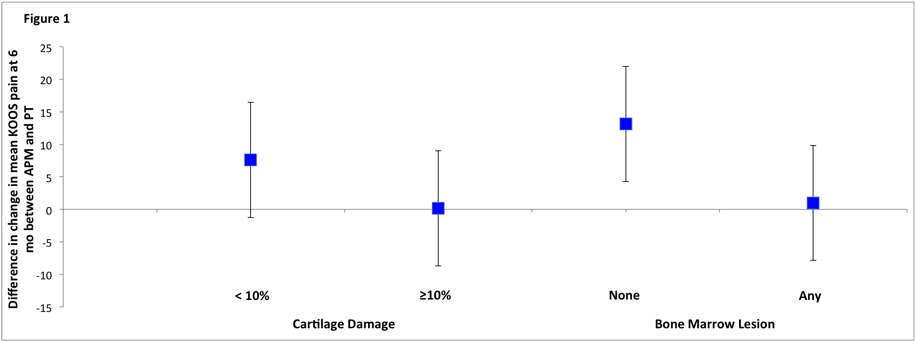
Results: The sample consisted of 223 knees (one per person); 129 (58%) had APM and 94 (42%) PT. The baseline KOOS Pain in all imaging categories ranged from 44-45 points. Patients with ≥10% cartilage damage had similar improvement in pain with PT and APM (23 points), while patients with <10% cartilage damage had greater improvement with APM than with PT (28 vs 20 points). Those with BML also had similar improvement with APM and PT (24 vs 23 points), while those with no BMLs had greater improvement with APM than with PT (29 vs 16 points). While these difference in efficacy of APM vs. PT were clinically relevant (MCID~8 points) they did not reach statistical significance. (p-value for interaction =0.17 for cartilage damage and 0.11 for BML).
Conclusion: These data suggest that for patients with more extensive baseline cartilage damage and BMLs there is no clinically meaningful difference in pain outcomes between management with APM vs. PT. However, though not statistically significant, our data suggest that patients with less cartilage damage and those with no BMLs at baseline may receive more symptomatic benefit from APM than from PT. These relationships should be pursued in larger cohorts to further assess the role of APM in management of meniscal tear in those with less cartilage damage or no BMLs.
| Table 1 | |||||
|
|
N (%) |
Baseline KOOS Pain, mean (SE) |
ΔKOOS Pain (95% CI) at 6 months |
||
|
APM |
PT |
P interaction |
|||
| Cartilage Damage |
|
||||
|
≥10% |
151 (68) |
45.8 (16.1) |
-23.2 (-27.2,-19.4) |
-23.1 (-27.5, -18.7) |
0.17
|
|
<10% |
69 (31) |
44.4 (16.0) |
-27.9 (-33.5,-22.4) |
-20.3 (-27.2, -13.4) |
|
| Bone Marrow lesion |
|
|
|
|
|
|
Any |
185 (85) |
45.3 (16.6) |
-23.9 (-27.5,-20.4) |
-22.9 (-26.9,-18.9) |
0.11 |
|
None |
33 (15) |
45.9 (13.1) |
-28.8 (-36.5,-21.2) |
-15.7 (-27.4, -4.0) |
|
| KOOS; Knee Injury and Osteoarthritis Outcome Score, SE; standard error, APM; arthroscopic partial meniscectomy, PT; physical therapy | |||||
Difference between APM and PT for change in KOOS Pain at 6 months for each imaging category with confidence intervals
To cite this abstract in AMA style:
MacFarlane L, Yang HY, Collins JE, Guermazi A, Jones M, Winter A, Losina E, Katz JN. Influence of Baseline Magnetic Resonance Imaging Features on Outcomes of Operative and Non-Operative Treatment of Meniscal Tear in Patients ≥ 45 [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/influence-of-baseline-magnetic-resonance-imaging-features-on-outcomes-of-operative-and-non-operative-treatment-of-meniscal-tear-in-patients-%e2%89%a5-45/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influence-of-baseline-magnetic-resonance-imaging-features-on-outcomes-of-operative-and-non-operative-treatment-of-meniscal-tear-in-patients-%e2%89%a5-45/