Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Absenteeism and work disability substantially contribute to the economic burden of psoriasis and psoriatic arthritis (PsA). This study compared work absenteeism and short-term disability among adults with psoriasis, PsA, and controls with neither psoriasis nor PsA in the United States.
Methods: Adults eligible for work absenteeism and/or short-term disability benefits between 1/1/2009 and 2/29/2020 were screened in the IBM MarketScan Commercial and Health and Productivity Management Databases. The following groups were defined: 1) Psoriasis: ≥ 1 inpatient or 2 outpatient psoriasis diagnoses and no PsA diagnoses; 2) PsA: ≥ 1 inpatient or 2 outpatient PsA diagnoses; 3) Control: absence of psoriasis and PsA diagnoses. Controls were matched 3:1 to psoriasis and PsA patients based on age, gender, and comorbidities. Absenteeism, short-term disability, and corresponding costs (in 2019 USD) were evaluated descriptively and through mixed models.
Results: 5,785 psoriasis and 1,245 PsA absentee-eligible and 35,512 psoriasis and 7,434 PsA short-term disability-eligible patients were matched to the control group. During the first year of follow-up, 9.7% of patients with PsA had short-term disability leave compared with 6.2% of patients with psoriasis and 4.8% of controls (Table 1). The odds of short-term disability at one year were significantly greater among patients with PsA than psoriasis (OR: 1.56, 95% CI: 1.45-1.69) and controls (OR: 1.95, 95% CI: 1.82-2.10). Average costs from non-recreational work absences were $1,891, $1,680, and $1,333 per patient per year for the PsA, psoriasis, and control group, respectively. Costs associated with non-recreational work absences and short-term disability were significantly greater for patients with PsA and patients with psoriasis than controls at one year (p< 0.0001 for all comparisons). These costs were also significantly greater for PsA than psoriasis at one year (p=0.001 and p< 0.0001, respectively). This trend of increased costs for patients with PsA compared with the other groups was sustained throughout the five years of follow-up (Figures 1 & 2).
Conclusion: Work absenteeism and short-term disability were greater among both the psoriasis and PsA groups than the control group. Absenteeism and short-term disability were greater among patients with PsA than psoriasis. These findings demonstrate the substantial impact that psoriatic disease has on patients’ work related outcomes, and highlight remaining unmet needs for patients with psoriatic disease.
 Table 1. Work absenteeism and short-term disability during follow up
Table 1. Work absenteeism and short-term disability during follow up
 Figure 1. Average costs from non-recreational hours missed from work per patient per year
Figure 1. Average costs from non-recreational hours missed from work per patient per year
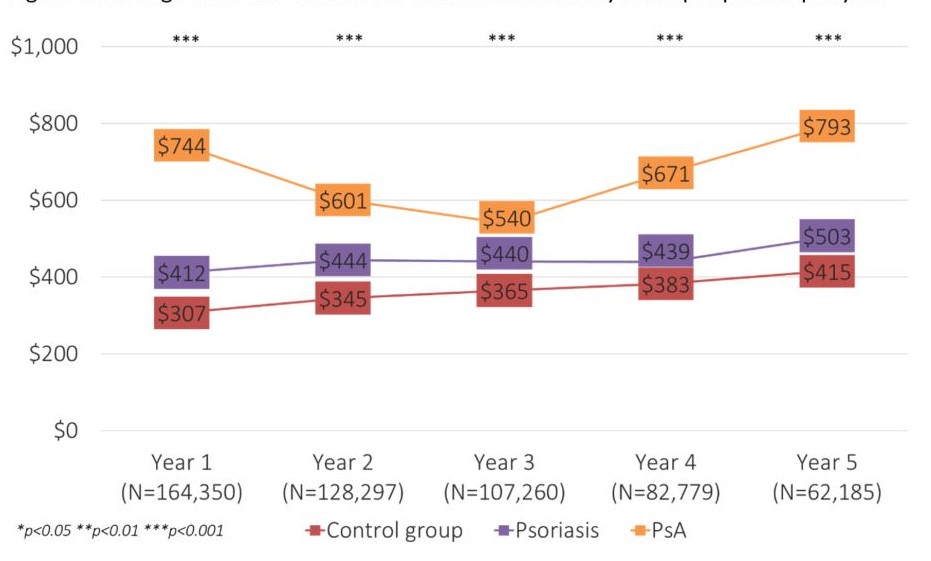 Figure 2. Average costs associated with short-term disability leave per patient per year
Figure 2. Average costs associated with short-term disability leave per patient per year
To cite this abstract in AMA style:
Orbai A, Reddy S, Peterson S, Dennis N, Villacorta R, Mesana L, Chakravarty S, Pacou M, Lin I, Baker T, Wang Y, Walsh J. Work Absenteeism and Disability Associated with Psoriatic Arthritis and Psoriasis in the United States – A Retrospective Study of Claims Data from 2009 to 2020 [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/work-absenteeism-and-disability-associated-with-psoriatic-arthritis-and-psoriasis-in-the-united-states-a-retrospective-study-of-claims-data-from-2009-to-2020/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/work-absenteeism-and-disability-associated-with-psoriatic-arthritis-and-psoriasis-in-the-united-states-a-retrospective-study-of-claims-data-from-2009-to-2020/
