Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Classification of patients as having axial spondyloarthritis (axSpA) by the imaging arm of the ASAS criteria relies partly on the detection of bone marrow edema (BME) suspicious of SpA on magnetic resonance imaging (MRI) of the sacroiliac joints (SIJ). Fatty lesions (FL) and erosions on SIJ-MRI have been suggested to be genuinely related to SpA in the context of interpretation of a ‘positive’ MRI in case of doubtful BME cases (1). We evaluated the role of different SIJ-MRI lesions for diagnosing axSpA in daily routine practice.
Methods: Consecutive patients with chronic back pain (duration >3 months) starting before age 45 and clinical suspicion of axSpA underwent a complete diagnostic workup including SIJ-MRI. All clinical, laboratory and imaging data were available to experienced rheumatologists for diagnosing axSpA or not (non-SpA). In parallel, two experienced readers, blinded to all patients´ information and diagnosis, evaluated the MRIs and made a ‘diagnostic judgement’ based only on imaging features. In addition, radiologists quantitatively assessed MRIs for BME (Berlin Score), FL, erosions, sclerosis and ankylosis.
Results: A total of 300 consecutive patients were recruited. AxSpA was diagnosed by the rheumatologists in 131 patients (43.7%) with mean age of 34.5±7.2 years, 73% HLA-B27+, mean symptom duration 58.6±69.5 months, vs. 169 non-SpA patients with mean age of 34.5±7.4 years, 21.3% HLA-B27+, mean symptom duration 33.9±45.1 months. The ASAS classification criteria were fulfilled by 99/131 patients diagnosed with axSpA (75.6%) vs. 70/169 patients diagnosed vs. non-SpA non-SpA (41.4%).
In 97/162 patients, rheumatologists and radiologists agreed on a diagnosis of axSpA and in the same number (97/162) there was agreement for non-SpA (overall agreement: 86.3%). However, 34/131 (28.1%) patients were diagnosed with axSpA by rheumatologists but not by radiologists.
According to radiologists, BME alone was critical for diagnosis in only 7/97 patients (7.2%) with axSpA as agreed by both, rheumatologists and radiologists, in contrast to chronic lesions alone (30/97, 30.9%) or the combination of both lesion types (60/97, 61.9%).
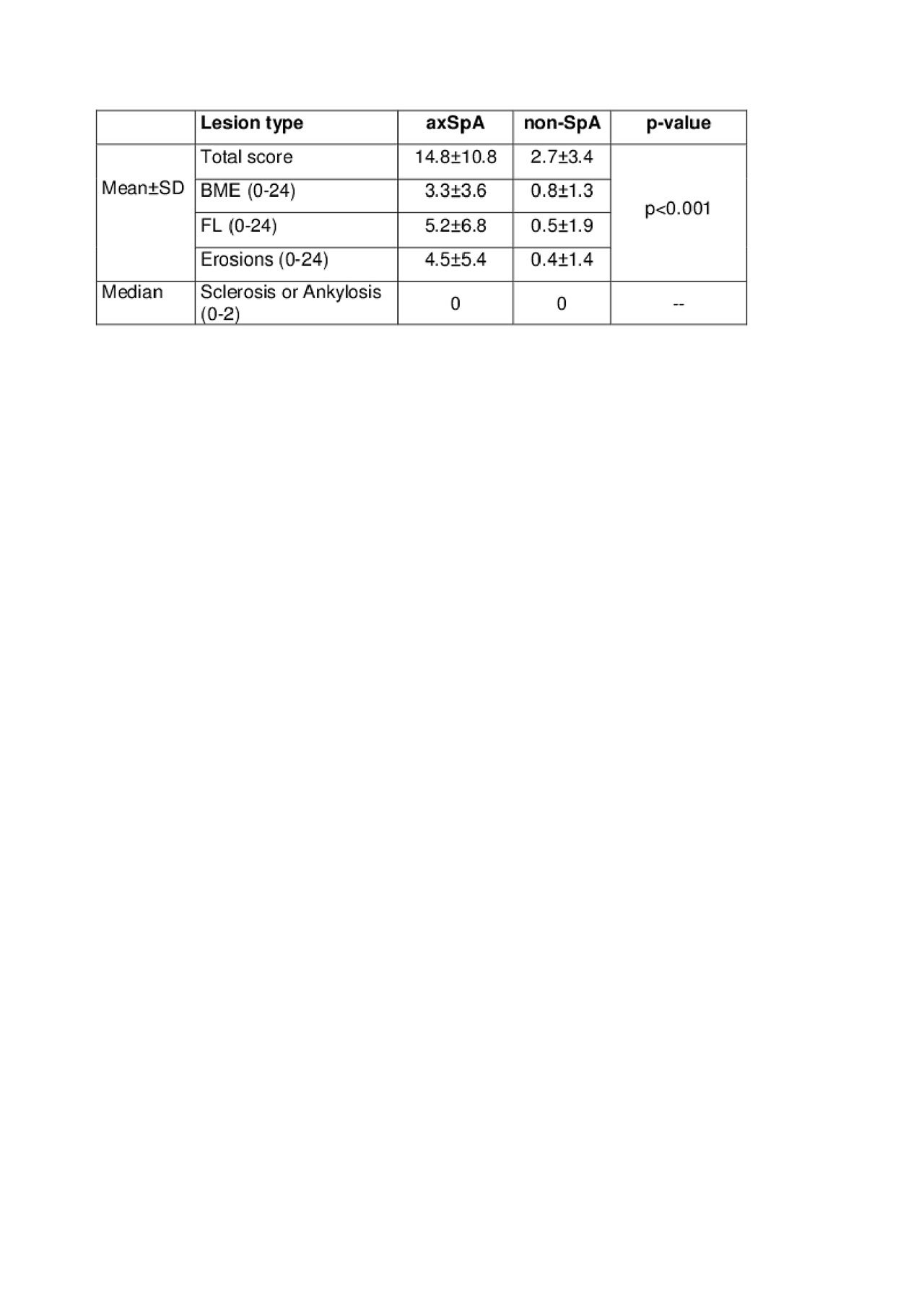
While the sensitivity of BME for diagnosing axSpA did not change, the specificity improved when chronic lesions were also present (Tab.1). In addition, based on rheumatologists´ diagnosis, the respective odds ratio (OR) for identifying axSpA by MRI was higher when chronic lesions were present (Tab.1). MRI scores were significantly higher in axSpA vs. non-SpA patients, indicating that axSpA is associated with deeper BME or chronic lesions (Tab.2).
Conclusion: The combination of structural changes and BME lesions as assessed by MRI performed best in the process of identifying axSpA in consecutive patients in a real-life setting. The discrepancy in diagnosis between rheumatologists and radiologists reflects the increasing insecurity of including only BME of SIJ as the major criterium for diagnosing axSpA.
References:
(1) Lambert R et al. Ann Rheum Dis 2016
To cite this abstract in AMA style:
Baraliakos X, Ghadir A, Fruth M, Kiltz U, Braun J. Which Magnetic Resonance Imaging Lesions of the Sacroiliac Joints Are of Diagnostic Value for Axial Spondyloarthritis? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/which-magnetic-resonance-imaging-lesions-of-the-sacroiliac-joints-are-of-diagnostic-value-for-axial-spondyloarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/which-magnetic-resonance-imaging-lesions-of-the-sacroiliac-joints-are-of-diagnostic-value-for-axial-spondyloarthritis/