Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: The diagnostic delay remains long in patients with spondyloarthritis (SpA), thus effective screening/referral strategies for early recognition are needed. Up to 40% of patients presenting with acute anterior uveitis (AAU) have an undiagnosed SpA [1]. The Dublin Uveitis Evaluation tool (DUET) was presented as a referral tool for ophthalmologists [1]. The objective of this study was to compare the performance of the DUET with a screening strategy based on the Assessment of SpondyloArthritis International Society (ASAS) referral recommendations in AAU patients (figure, [2]).
[1] Haroon M, et al. Ann Rheum Dis 2015;74:1990-5.
[2] Poddubnyy D, et al. Ann Rheum Dis 2015;74:1483-7.
Methods: A total of 207 consecutive patients with non-infectious AAU seen in the ophthalmology clinic and ophthalmological private practices were included, 189 of them completed a standardized rheumatological examination in the specialized center including imaging of sacroiliac joints (MRI performed in 185 patients, X-rays performed in 116 patients) allowing for a definite conclusion on the presence/absence of SpA. The sensitivity, specificity and positive predictive value of both referral tools were calculated. Mann Whitney U and Fisher’s exact tests were used for comparison between AAU patients with and without SpA.
Results: Out of the 189 AAU patients, 105 (56%) were diagnosed with SpA: the majority of them (n=100, 95%) had predominantly axial SpA, 5 patients solely peripheral SpA. 33 of the included 189 patients had a previous external diagnosis of SpA, however, in three out of them SpA was excluded after rheumatologist evaluation as part of the study.
Patients with underlying SpA were more often male, HLA-B27 positive and had predominantly unilateral uveitis (table 1). Though back pain was frequent in the overall study population, back pain present at inclusion as well as inflammatory back pain were significantly more prevalent in the AAU patients with SpA. Moreover, SpA patients had higher disease activity parameters and elevated inflammatory markers (both CRP and ESR) as well as reduced spinal mobility compared to patients without SpA. Patients with SpA presented more frequently with psoriasis and peripheral arthritis.
The ASAS referral tool showed a higher sensitivity (86% vs. 83%) but a lower specificity (28% vs. 41%) compared to the DUET. The positive predictive value was 58% for the ASAS tool and 62% for the DUET (table 2). Similar performances were observed when analyzing only patients without a known diagnosis of SpA (table 2).
Conclusion: We revealed a high prevalence of undiagnosed SpA in patients with acute anterior uveitis. As anticipated, the DUET strategy also including psoriasis and HLA-B27 positivity showed higher specificity for recognition of SpA than the ASAS referral tool focusing on back pain, which showed a higher sensitivity. Given the high prevalence of SpA in AAU patients, we recommend referring all AAU patients with relevant back pain for a rheumatologic evaluation.
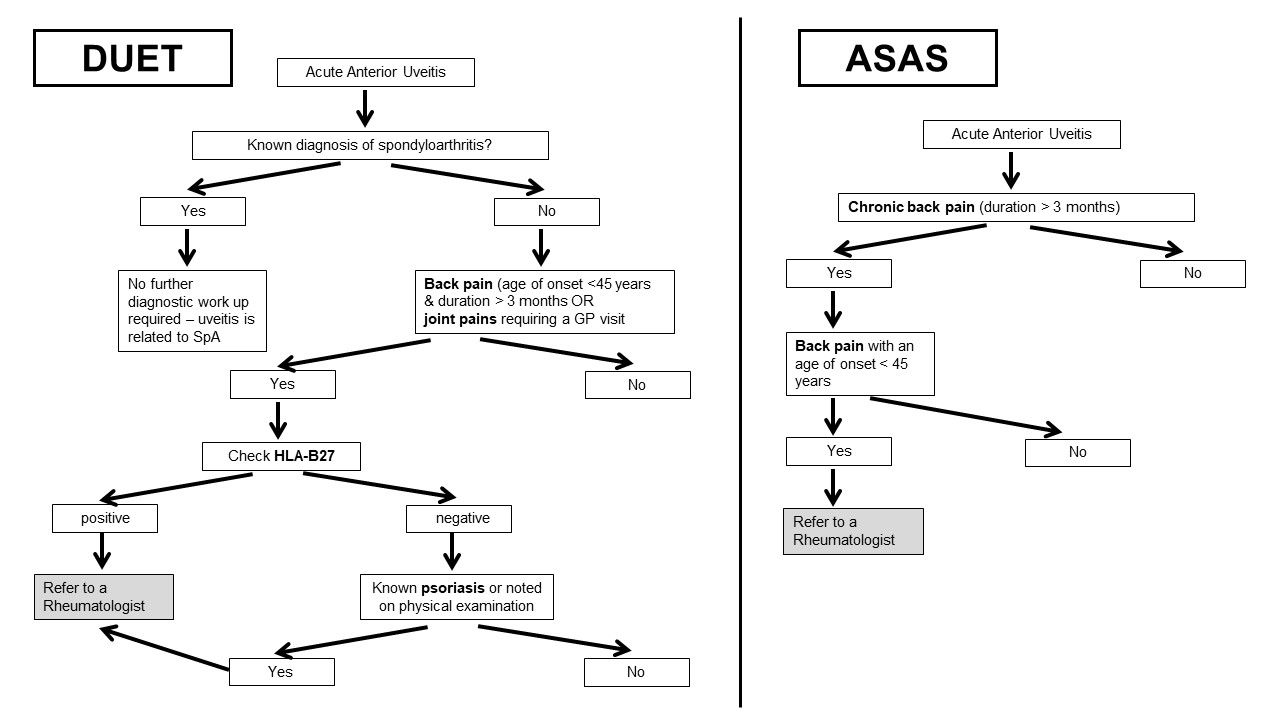 Figure: DUET and ASAS referral tool, modified after [1,2].
Figure: DUET and ASAS referral tool, modified after [1,2].
 Table 1. Demographic and clinical parameters of the 189 included patients with acute anterior uveitis with and without spondyloarthritis (SpA). * Mann Whitney U test for numerical and Fisher’s exact test for categorical variables. Mean is given for numerical variables together with standard deviation (SD).
Table 1. Demographic and clinical parameters of the 189 included patients with acute anterior uveitis with and without spondyloarthritis (SpA). * Mann Whitney U test for numerical and Fisher’s exact test for categorical variables. Mean is given for numerical variables together with standard deviation (SD).
 Table 2. Performance of referral tools in all patients (Nf180) and only patients without a previously diagnosed spondyloarthritis (Nf148): Dublin Uveitis Evaluation Tool (DUET) versus an adaption of the Assessment of SpondyloArthritis International Society referral tool (ASAS).
Table 2. Performance of referral tools in all patients (Nf180) and only patients without a previously diagnosed spondyloarthritis (Nf148): Dublin Uveitis Evaluation Tool (DUET) versus an adaption of the Assessment of SpondyloArthritis International Society referral tool (ASAS).
To cite this abstract in AMA style:
Rademacher J, Müllner H, Pohlmann D, Rios Rodriguez V, Proft F, Protopopov M, Lüders S, Muche B, Spiller L, Weber A, Sron S, Haibel H, Pleyer U, Poddubnyy D. What Is the Optimal Screening Strategy for Early Recognition of Spondyloarthritis in Patients with Acute Anterior Uveitis? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/what-is-the-optimal-screening-strategy-for-early-recognition-of-spondyloarthritis-in-patients-with-acute-anterior-uveitis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/what-is-the-optimal-screening-strategy-for-early-recognition-of-spondyloarthritis-in-patients-with-acute-anterior-uveitis/
