Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Classification criteria for axSpA comprise an imaging and a clinical arm, the former requiring radiographic or MRI evidence of sacroiliitis. Several cohorts have reported the performance of the ASAS classification criteria in settings where clinical, radiographic, and MRI features have been simultaneously incorporated into the diagnostic evaluation in arriving at a gold standard for the testing of the criteria, which introduces circularity. We aimed to test the performance of the criteria in a setting where diagnostic evaluation can be conducted sequentially before and after MRI assessment in unselected patients referred with undiagnosed back pain who have presented with acute anterior uveitis (AAU), psoriasis, or colitis to their respective specialists.
Methods: Consecutive patients ≤45 years of age with ≥3 months undiagnosed back pain with any one of psoriasis, acute anterior uveitis (AAU), or colitis undergo routine clinical evaluation by a rheumatologist for axial SpA and MRI evaluation is ordered per rheumatologist decision. The rheumatologist determines the presence or absence of axial SpA and the degree of confidence in the diagnosis (-10 (definitely not SpA) to +10 (definite SpA)) at 3 sequential stages: 1. After the clinical evaluation; 2. After the results of labs (B27, CRP) and radiography; 3. After the results of MRI evaluation. We calculated the sensitivity and specificity of the ASAS criteria and the component imaging and clinical arms using the stage 2 (pre-MRI) and 3 (post-MRI) diagnostic assessments by the local rheumatologist as gold standard.
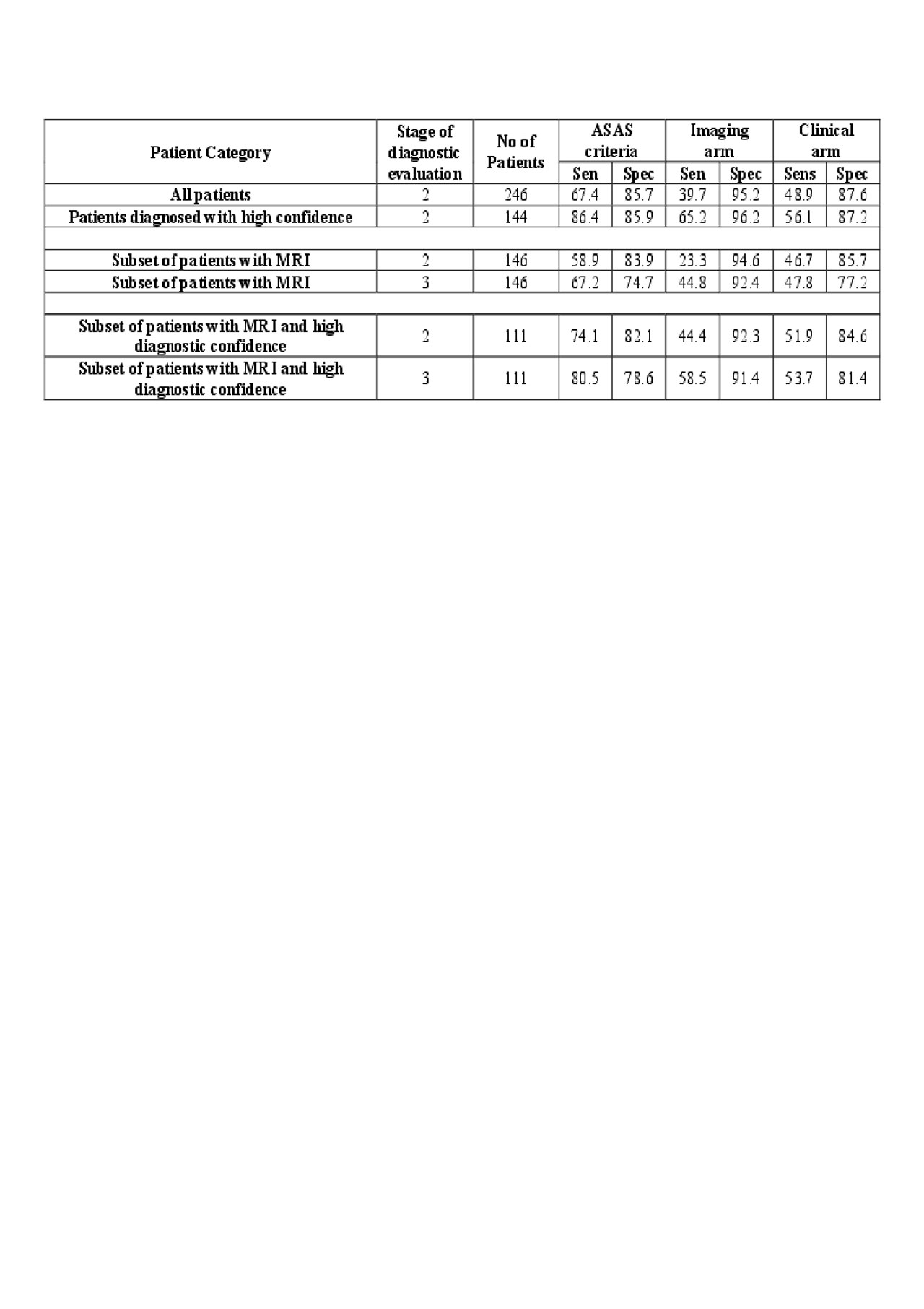
Results: A total of 246 patients were recruited, 47.6% being diagnosed with axSpA (61.5% male, age 33.7 years, symptom duration 7.6 years, B27 positive 52.1%), after final diagnostic evaluation. Sensitivity/specificity of the ASAS criteria, imaging arm, clinical arm after stage 2 diagnostic evaluation for the entire cohort (prior to assessment of MRI) were 67.4/85.7%, 39.7/95.2%, 48.9/87.6%, respectively (Table). Sensitivity and specificity were higher in patients diagnosed with a high degree of confidence. For the subset of 146 patients who had MRI evaluation, and therefore had diagnostic evaluation at both stage 2 (pre-MRI) and stage 3 (post-MRI evaluation), there was a substantial enhancement in the sensitivity of the imaging arm (from 23.3% pre-MRI to 44.8% post-MRI) without change in specificity ( >90%). However, there was a substantial decrease in specificity of the overall ASAS criteria from 83.9% pre-MRI to 74.7% post-MRI. This was primarily due to a substantial decrease in the specificity of the clinical arm from 85.7% pre-MRI to 77.2% post-MRI.
Conclusion: xThe clinical arm of the ASAS criteria performed less well after MRI assessment was added to the process of evaluation to enhance diagnostic precision. This could reflect rheumatologist diagnostic ‘over-call’ based on clinical findings in a population presenting with a higher pre-test probability of axSpA.
To cite this abstract in AMA style:
Maksymowych W, Carmona R, Chan J, Yeung J, Aydin S, Martin L, Masetto A, Mosher D, Ziouzina O, Keeling S, Rohekar S, Dadashova R, Paschke J, Carapellucci A, Lambert R. What Is the Impact of MRI on the Performance of the ASAS Classification Criteria in Patients Presenting with Undiagnosed Back Pain? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/what-is-the-impact-of-mri-on-the-performance-of-the-asas-classification-criteria-in-patients-presenting-with-undiagnosed-back-pain/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/what-is-the-impact-of-mri-on-the-performance-of-the-asas-classification-criteria-in-patients-presenting-with-undiagnosed-back-pain/