Session Information
Date: Monday, November 9, 2020
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The purpose of this study was to characterize the frequency of visual ischemia (VI) as a manifestation of relapse or during follow-up in patients with GCA through performance of a systematic literature review.
Methods: Potentially eligible studies were identified from Medline and EMBASE databases from inception to November 31, 2019 using a search strategy that comprised of terms for “giant cell arteritis,” “temporal arteritis,” or “Horton’s disease,” with “relapse,” “recurrence,” “flare,” “outcome,” “follow-up,” or “prognosis.” VI was defined as transient or permanent, full or partial, monocular or binocular visual field loss. VI occurring within 4 weeks of GCA diagnosis was considered due to active disease and not included as a relapse event. Inclusion criteria used: (1) original research reported in English, (2) GCA definition provided, (3) VI outcome described as one of the following: (a) relapse rate/frequency denoting the presence or absence of VI, or (b) absolute number of VI events ( > 4 weeks after GCA diagnosis) even if total cohort relapse rate/frequency was not provided. In order to reduce bias from under-reporting of negative results, studies that reported relapse rates/frequencies with accompanying relapse characteristics but did not provide initial detail regarding the presence/absence of VI were also identified. In such circumstances, the primary authors were directly contacted for patient-level data regarding VI and these studies were included in the final analysis if such data were available and provided.
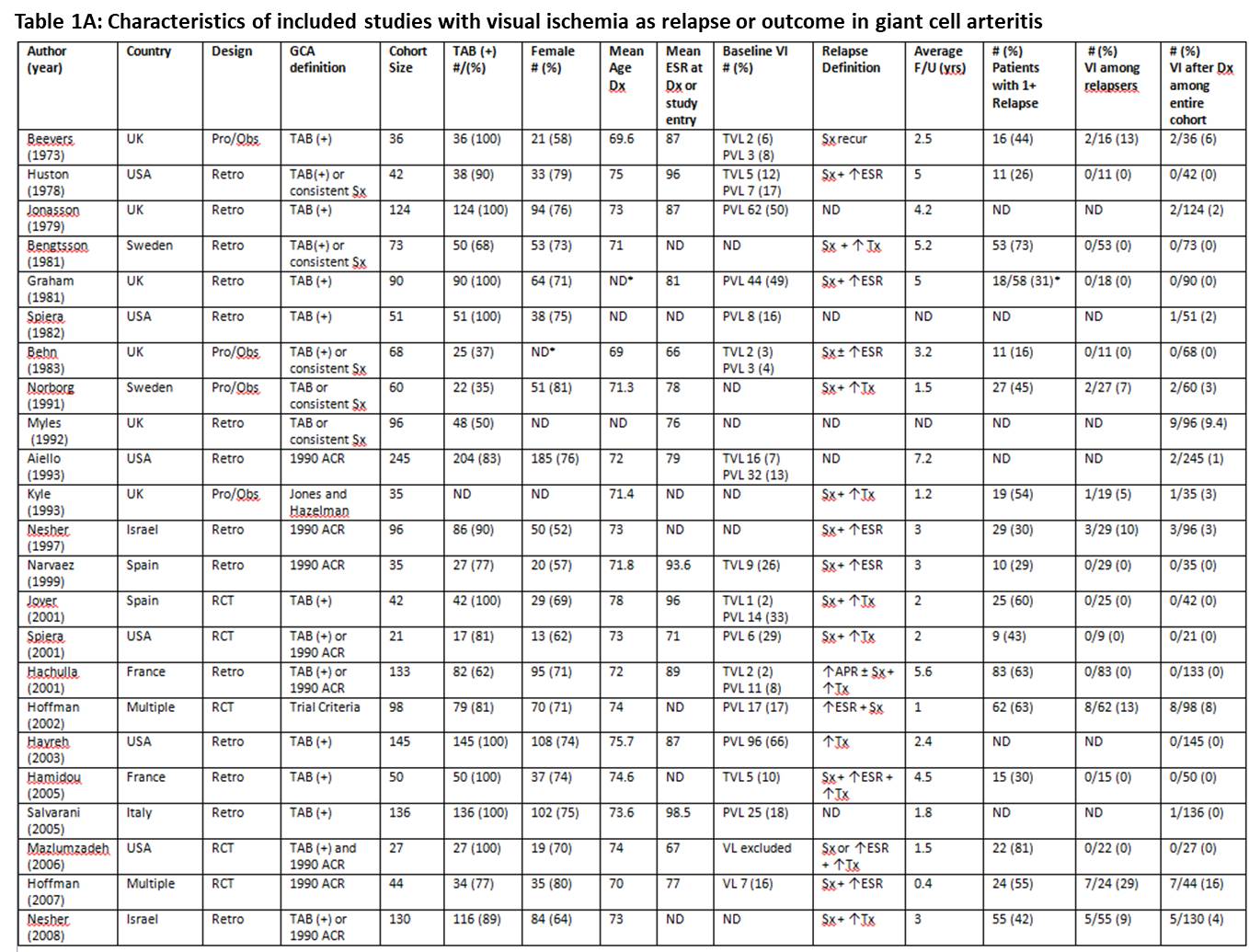
Results: A total of 913 unique articles were identified and underwent screening (K.B. and M.J.K). Among these, 148 articles underwent independent full-text review by two physicians (K.B. and M.J.K). 33 articles met full inclusion criteria and an additional 21 articles included data on relapse but did not report VI patient data in the publication. Responses were received from authors of 11 of these 21 studies allowing for inclusion. 44 studies accounting for 3,649 patients with GCA were identified (Table 1). Average percentage of baseline VI was 19% (range 0-66%). The average length of follow-up was 3.4 years (range 0.4 to 8.7). VI developing > 4 weeks after GCA diagnosis was recorded in a total of 53 patients (1.5%).
Study-defined relapses were reported in 36 studies. A total of 1,215 patients with at least one or more relapses were recorded among 2,592 patients under observation (47%). Among these 36 studies, VI occurred in 37 patients (3.0%) with at least one study defined relapse event.
Comparing trial design, retrospective studies (n=25) reported 27 of 2,718 (1%) patients developed VI during follow-up whereas 19 of 541 (3.5%) patients in randomized controlled trials (n=8) developed VI during the trial or post-trial follow-up (Table 2).
Conclusion: This report outlines the first systematic review evaluating VI as a manifestation of relapse and during follow-up in GCA. Overall, VI > 4 weeks after GCA diagnosis is uncommon (1.5%) but is noted in up to 3% of patients with at least one relapse event. Frequencies of reported VI were 3.5 times higher in randomized controlled trials compared to retrospective studies.
To cite this abstract in AMA style:
Bugdayli K, Ungprasert P, Warrington K, Koster M. Visual Ischemia During Relapse and Follow-up of Giant Cell Arteritis: A Systematic Review [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/visual-ischemia-during-relapse-and-follow-up-of-giant-cell-arteritis-a-systematic-review/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/visual-ischemia-during-relapse-and-follow-up-of-giant-cell-arteritis-a-systematic-review/