Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid syndrome (APS) is a thrombo-inflammatory disease propelled by autoantibodies that recognize cell surface phospholipids and phospholipid binding proteins. The result is an increased risk of thrombotic events, pregnancy morbidity, and various other autoimmune and inflammatory complications. Vascular liver disorders (VLD), such as portal vein thrombosis, Budd-Chiari syndrome and porto-sinusoidal vascular disorder, are rare but often related to an underlying hypercoagulable state. We aimed to describe the clinical and immunological features of VLD in APS patients.
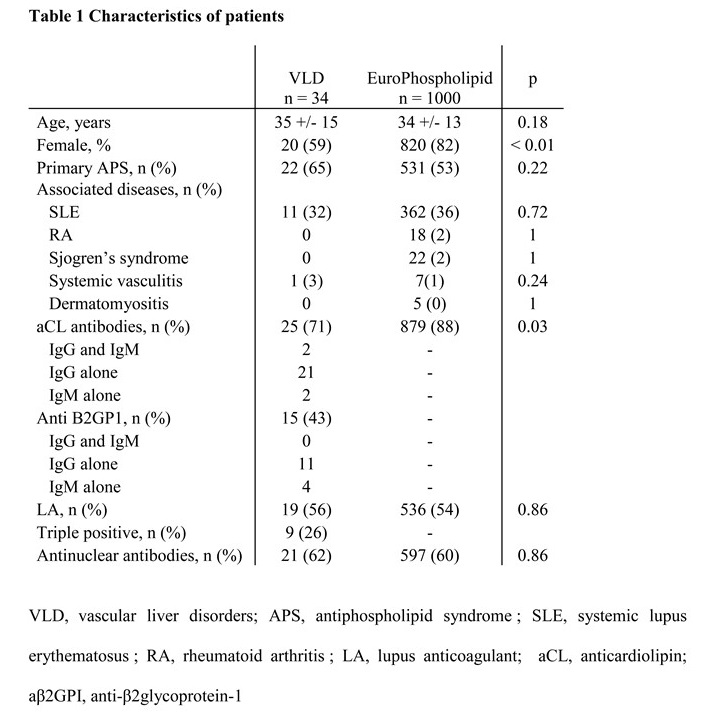
Methods: The study is a national, multicentric, retrospective study involving APS patients (2006 Miyakis criteria) followed in 4 French tertiary university centers including 3 national referral centers for rare autoimmune diseases. Clinical and serological data of APS patients with VLD were analyzed and compared with patients included in the EuroPhospholipid cohort.
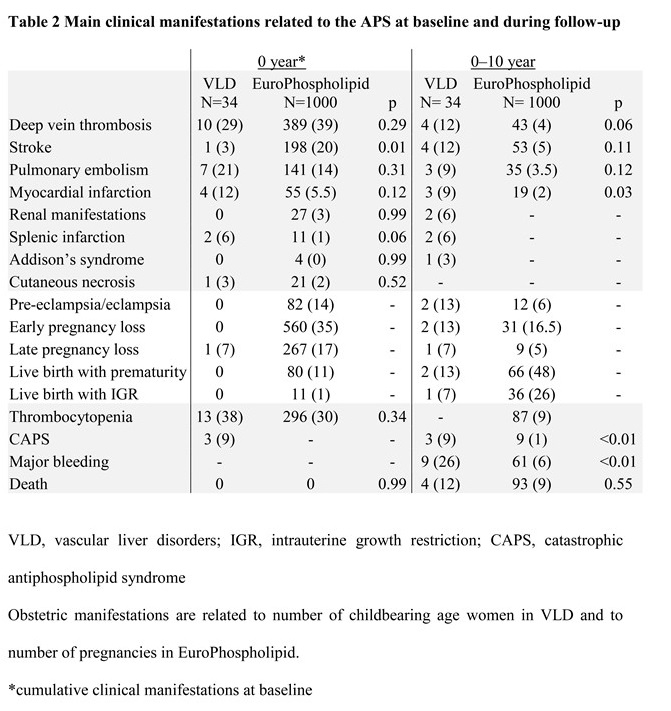
Results: Thirty-four APS patients with VLD (20 women (59%); median (IQR) age 35 (24.5;42) years at APS diagnosis; 65% of primary APS) were included in the study. Forty-one VLD were reported in 34 patients including portal vein thrombosis (n=26/41, 63%), Budd-Chiari syndrome (n=12/41, 29%) and porto-sinusoidal vascular disorder (n=3/41, 7%). VLD were the first thrombotic event in 27 (79%) patients. In patients in whom VLD was the heralding manifestation of APS, APS diagnosis was made at VLD onset (n=18/27, 67%) or a median (IQR) of 6 (3;7) years after (n=9/27, 33%), when a second thrombotic event occurred. Lupus anticoagulant, IgG/IgM anticardiolipin and IgG/IgM anti-β2glycoprotein-1 autoantibodies were detected in 56%, 71% and 43% of patients, respectively and 26 % of patients were aPL triple-positive. All patients were treated with oral anticoagulants including VKA in all but one case. Over a median (IQR) of 9.5 (5;14) years of follow-up, 21 (62%) patients displayed a new thrombotic event while all but 2 (n=19/21, 90%) were under oral anticoagulants. Nine (26%) patients suffered major bleeding including digestive hemorrhage in 5 cases. Portal hypertension was documented in 15 (44%) patients. As compared with EuroPhospholipid APS patients (mean age of 34 (+/-13) years at disease onset), APS patients with VLD were more frequently male (n=14/34, 41% vs n=180/1000, 18%, p=0.002) and suffered a higher frequency of thrombotic recurrence (n=21/34, 62% vs n=118/771, 15%; p< 0.001) and major bleeding (n=9/34, 26% vs n=61/1000, 6%; p< 0.001) during follow up
Conclusion: VLD, mostly portal vein thrombosis, may be the presenting manifestation of APS. APS patients with VLD displayed a more severe thrombotic phenotype and are at higher risk of major bleeding.
To cite this abstract in AMA style:
Katims M, Pineton de Chambrun M, Yelnik C, Mageau A, Clarke A, Papo M, Amoura Z, Lambert M, Papo T, Delaval L, Rautou P, Costedoat-chalumeau N, Sacré K. Vascular Liver Disorders in Patients with Antiphospholipid Syndrome: A Retrospective National Multicentre Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/vascular-liver-disorders-in-patients-with-antiphospholipid-syndrome-a-retrospective-national-multicentre-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vascular-liver-disorders-in-patients-with-antiphospholipid-syndrome-a-retrospective-national-multicentre-study/