Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Disparities in pregnancy outcomes among women with SLE remain understudied, with few available racially-diverse datasets. We previously validated algorithms to identify pregnancies in women with SLE within the electronic medical record (EMR) of tertiary care centers in the Southern United States, finding the algorithms more accurate for Black than White women with SLE: there was a high rate of SLE over-labeling in White women, particularly by physicians other than rheumatologists. In this study, we analyzed differences in pregnancy outcomes based on different algorithm definitions of SLE pregnancies in Black and White patients with SLE.
Methods: Using the Common Data Model EMR-based datasets within the Carolinas Collaborative (Sites A, B, and C), we identified women with pregnancy delivery data (2014-2019) and ≥1 SLE ICD9/10 code. From this dataset, we identified four cohorts of SLE pregnancies, 3 using different algorithms and one via chart review to confirm SLE diagnosis. We compared the pregnancy outcomes identified in each of these cohorts for Black and White women. All pregnancies identified using the sensitive algorithm from Sites A and B were included in the chart review; chart review was not possible for Site C data.
Sensitive algorithm: 1 ICD-9/10 code for SLE prior to delivery.
Predictive algorithm: ≥4 ICD9/10 codes + HCQ for SLE.
XG Boost: a machine learning-derived algorithm validated for Black and White women with SLE.
Confirmed: Chart reviewed for SLE.
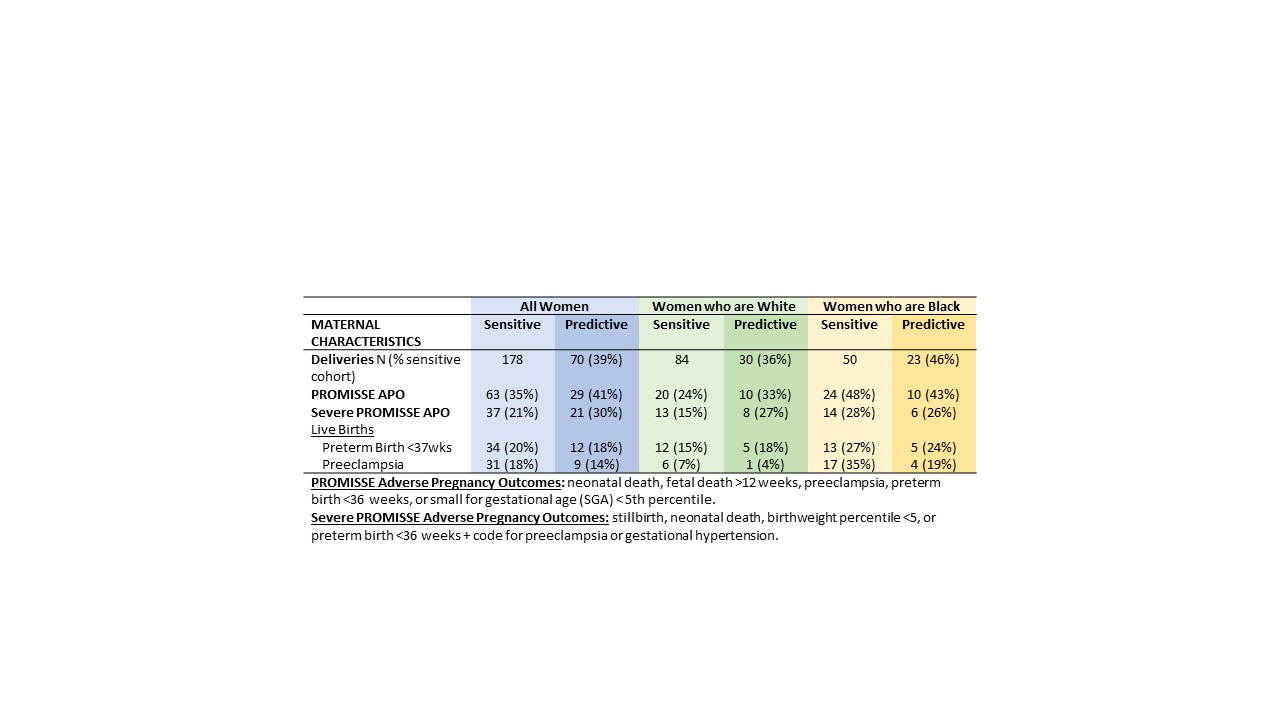
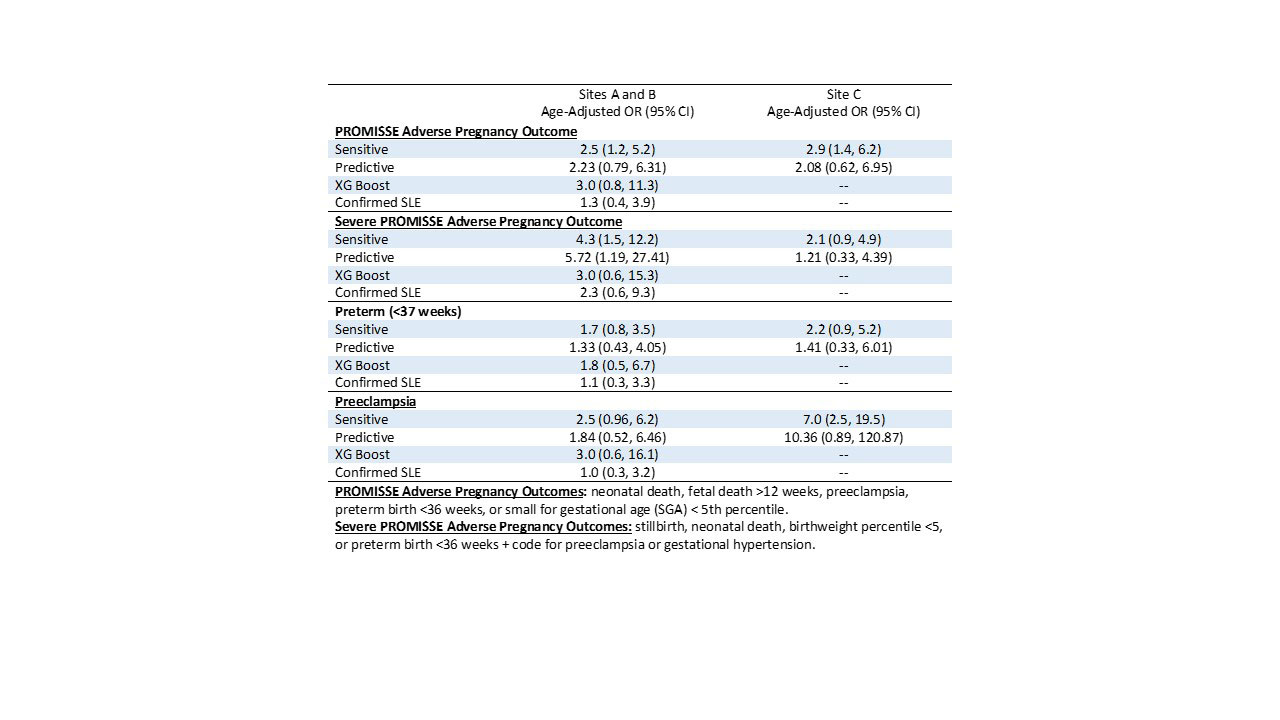
Results: Of 172 pregnancies in women with ≥1 SLE ICD9/10 code (Sensitive algorithm, sites A & B), 55% had SLE by the Predictive algorithm (44% of White and 61% of Black women), 53% by the XG Boost algorithm (34% of White and 65% of Black women), and 49% had SLE confirmed by chart review (34% of White and 62% of Black women). Overall, adverse pregnancy outcomes occurred in 40% of pregnancies in women with ≥1 ICD9/10 SLE code and 52% of pregnancies with confirmed SLE (Figure 1 for Sites A&B and Table 1 for Site C). SLE was frequently over-diagnosed in women who were White, resulting in 40-75% lower rates of adverse pregnancy outcomes in cohorts identified using algorithms vs. the confirmed cohort. Over-diagnosis of SLE was less common for Black women resulting in pregnancy outcomes 12-20% lower in algorithm-derived vs. confirmed SLE cohorts. While the EMR algorithms suggested significantly higher rates of adverse pregnancy outcomes in Black than White women, these disparities were smaller and no longer significant in the cohorts of women confirmed through chart review (Table 2).
Conclusion: Within these university hospitals in the southeastern US, pregnancy outcomes for Black and White women with confirmed SLE were similar. The over-diagnosis of SLE in White women led the algorithms to include women without SLE, which caused large under-estimations of their pregnancy risk. As Black women in this study were more accurately labeled for SLE, the algorithms identified more accurate estimates of pregnancy risk. This study suggests that race-based differences in algorithm performance can impact our understanding of racial disparities in SLE.
To cite this abstract in AMA style:
Clowse M, Oates J, Kirchoff K, Barnado A, Sheikh S, Crofford L, Eudy A. Variability in Racial Disparities in Pregnancy Outcomes in Women with SLE by Diagnosis Algorithm [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/variability-in-racial-disparities-in-pregnancy-outcomes-in-women-with-sle-by-diagnosis-algorithm/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/variability-in-racial-disparities-in-pregnancy-outcomes-in-women-with-sle-by-diagnosis-algorithm/