Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: MRI can detect both inflammatory and structural lesions in the sacroiliac joints (SIJ) of patients with axial SpA. However, standard MRI sequences do not directly depict bone and the appearance of erosion may vary according to the presence/absence of inflammation. Consequently, further validation using an accepted gold standard, namely, computed tomography (CT), is essential. We aimed to assess the detection of structural lesions of bone in the SIJ by MRI using CT as the gold standard.
Methods: CT scans from 44 patients (26 females, mean age 49.4 years, mean symptom duration 9.1 years) were reconstructed in the semicoronal plane parallel to the superior border of the sacrum, as for conventional MRI evaluation of the SIJ, and scoring of lesions by CT was confined to this plane. Structural lesions were scored in consecutive slices in SIJ quadrants (erosion, sclerosis) or SIJ halves (ankylosis) on a dichotomous basis (present/absent) using the same anatomical principles for defining SIJ quadrants as developed for the SPARCC MRI SIJ inflammation and structural scores. Consecutive semicoronal slices from T1W MRI scans of the SIJ from the same cases conducted at the same time as CT were assessed independently for structural lesions (erosion, fat, backfill, ankylosis, sclerosis) blinded to CT assessments using the MORPHO modification of the SPARCC method. MRI lesions were defined according to the Canada-Denmark MRI group. An online scoring module recorded detailed scores for individual SIJ slices. Agreement between CT and MRI was assessed by kappa statistics. Sensitivity/specificity of MRI for CT lesions was calculated. The primary analysis was based on lesions detected concordantly by both readers at the level of the individual iliac/sacral joint surface (erosion, sclerosis) or the individual joint (ankylosis, backfill).
Results: With CT as gold standard and a lesion defined as being present when recorded in the same location on at least 1 coronal slice by both readers, MRI-defined ankylosis had 56.3% sensitivity and 100% specificity for CT ankylosis (Table). For erosion, sensitivity and specificity of MRI was 81.3% and 96.2%, and for sclerosis, sensitivity and specificity of MRI was 50% and 97%, respectively. Agreement between CT and MRI for erosion increased when the cut-off for presence of a lesion was set at 2 slices but only marginally for sclerosis, even when the cut-off for presence of a lesion was set at 3 slices. Lesions observed on CT corresponding to backfill on MRI were ankylosis, erosion, and sclerosis, in 66.7%, 66.7%, and 80% of backfill lesions, respectively.
Conclusion: Ankylosis and erosion on MRI correspond closely with the same type of lesion observed on CT. Both new bone formation and erosion are frequently evident on CT at locations where backfill is observed on MRI supporting the hypothesis that backfill is an intermediary tissue between erosion and ankylosis. 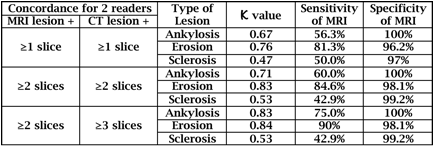
To cite this abstract in AMA style:
Lambert RG, Loeuille D, Raynal M, Melchior J, D'Agostino MA, Paschke J, Maksymowych W. Validation of MRI Structural Lesions Using Computed Tomography in Patients with Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/validation-of-mri-structural-lesions-using-computed-tomography-in-patients-with-axial-spondyloarthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/validation-of-mri-structural-lesions-using-computed-tomography-in-patients-with-axial-spondyloarthritis/
