Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Uveitis is a frequent extraarticular manifestation of axial Spondyloarthritis (axSpA), specifically anterior uveitis. Effects of biological therapy on uveitis associated to axSpA are poorly understood. Our objetive is to assess in axSpA a) the frequency of uveitis and clinical features; b) its association with axSpA activity, the impact of disease and functional disability, c) effectiveness of synthetic disease-modifying drugs and biological therapy and, d) frequency of ocular surface pathology.
Methods: A retrospective longitudinal study from a cohort of 309 unselected patients with axSpA classified according to the Assessment of SpondyloArthritis International Society criteria. All patients were diagnosed and managed uniformly in a single university centre. Uveitis was diagnosed by ophthalmologist. Sociodemographic data, clinical features, disease activity and treatments were collected. Incidence of uveitis was calculated before and after treatments initiation, reported as exposure adjusted incidence rate (EAIR) per 100 patient-years of biological drug exposure.
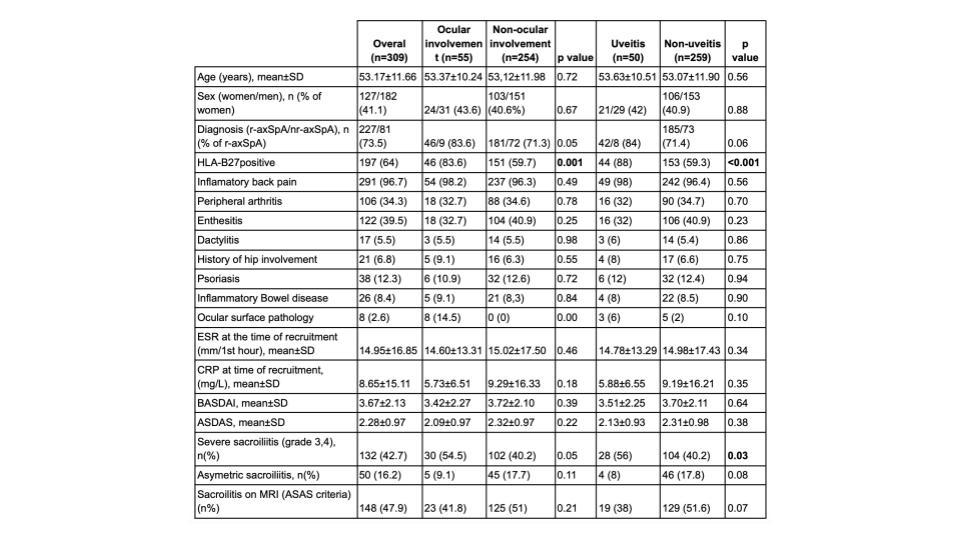
Results: Uveitis was observed in 50 patients (21 women/29 men) out of 309 (16.2%) and ocular surface pathology in 8 (2.7%). Demographic and clinical features in patients who developed ocular pathology and specifically uveitis and those who did not are summarized in Table 1. Uveitis was acute in all cases, anterior (98%), unilateral (72%), unilateral alternate (28%) and recurrent (70%). Ocular surface pathology was episcleritis (75%), scleritis (12.5%) and corneal ulcer (12.5%). Patients with uveitis had a greater frequency of positive HLA-B27 (88% p< 0.001) and severe sacroilitis (56% p=0.03) than patients without uveitis. Activity indexes (BASDAI, ASDAS) were similar regardless ocular involvement. Biological DMARDs were used in 24 (48%) patients with uveitis; 22(44%) of them received anti-TNFα monoclonal antibodies, etanercept (ETN) 4 (2%), secukinumab (SECU) 12 (24%) and JAK inhibitors (JAKi) 7 (14%).
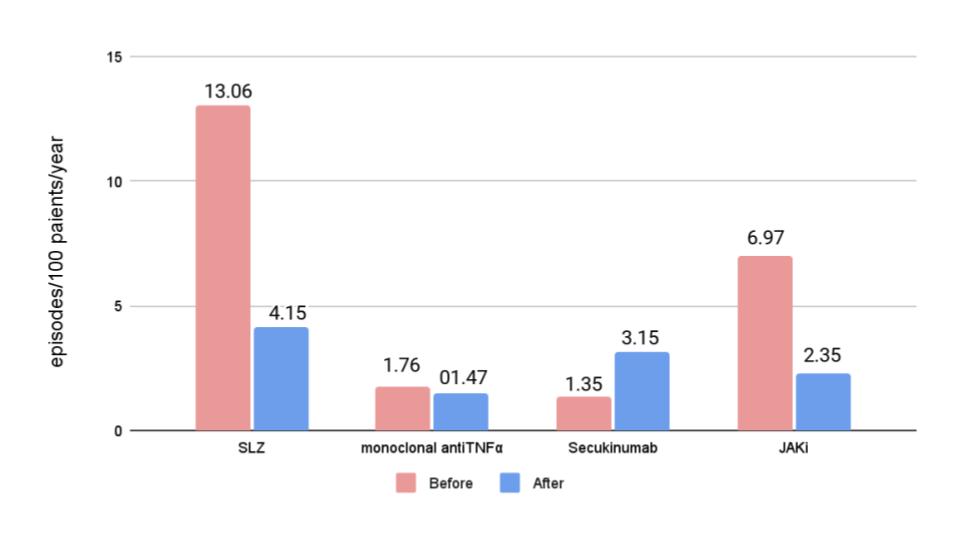
The EAIR of uveitis before treatment with sulfasalazine (SLZ) was 13.06 episodes/100 patients-year, with monoclonal anti-TNFα developed 1.76 episodes/100 patients-year, with SECU 1.35 episodes/100 patients/year and with JAKi 6.97 episodes/100 patients/year. After treatment, patients treated with SLZ, monoclonal anti-TNFα and JAKi developed 4.15, 1.47 and 2.35 episodes/100 patients/years, respectively, while in those treated with SECU was 3.15 episodes/100 patients/year.
Conclusion: Uveitis was observed in 16.2% of axSpA, while ocular pathology surface in 2.7%. Most patients with uveitis had positive HLA-B27 and severe sacroilitis in x-ray was more frequent. The most frequent pattern of uveitis observed in axSpA was acute, anterior and unilateral. The uveitis exposure adjusted incidence rate decreased with SLZ, antiTNFα monoclonal antibodies and JAKi and increased with SECU.
To cite this abstract in AMA style:
Martin-Sierra L, Sanchez Bilbao L, Rueda Gotor J, Calvo-Rio V, Egea-Fuentes A, Herrero-Morant A, Gonzalez-Mazon I, Muñoz-Rodriguez J, Blanco-Alonso R. Uveitis in Axial Spondyloarthritis: Study of 309 Patients in a Single University Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/uveitis-in-axial-spondyloarthritis-study-of-309-patients-in-a-single-university-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uveitis-in-axial-spondyloarthritis-study-of-309-patients-in-a-single-university-center/