Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Uveitis is the most common ocular manifestation of psoriatic arthritis (PsA). It has been described that uveitis in PsA tends to be insidious, chronic, posterior and bilateral onset, unlike uveitis in spondyloarthritis (SpA), which tends to be of sudden onset, acute course, unilateral and recurring. The use of TNF inhibitory agents (TNFi), especially monoclonal antibodies, has been shown to be effective in the prevention and treatment of refractory non-infectious uveitis.
In a large unselected series of patients with PsA, our objectives were to evaluate a) the epidemiology and clinical characteristics of uveitis associated with PsA, b) the differences between patients with and without uveitis and c)the relationship of uveitis with the biological treatment used.
Methods: Cross-sectional study of patients with PsA from a single referral hospital. They were classified according to the CASPAR criteria. Those with ocular manifestations were evaluated by expert ophthalmologists for the presence of uveitis. Demographic characteristics, clinical findings, complementary tests, presence of other extra-articular manifestations and treatment used were recorded.
Results: We studied 406 (202 women/204 men) patients with PsA; mean age of 46.3±12.3 years. The mean duration of the disease was 9.9±8.2 years.
Uveitis was observed in 20 of 406 (4.9%) patients (12 women/8 men); mean age of 43.1±14.5 years). Uveitis was characterized by being of acute onset (100%), anterior (80%), unilateral (80%) and recurrent (50%).
The comparison between patients with PsA who developed uveitis and those who did not is shown in the Table. The patients who present uveitis were characterized by a higher frequency of HLA-B27 (45%), sacroiliitis on MRI (25%) and ocular surface pathology (10%). The result of PsAID (Psoriatic Arthritis Impact of Disease) (median 5.9 [IQR 2.1-6.8]) and the BASFI index (Bath Ankylosing Spondylitis Functional Index) (median 4 [IQR 1.6-5]) was higher in patients with PsA and uveitis.
The incidence of uveitis prior to treatment with monoclonal antibodies TNFi and ETN was 56.3 and 6.03 episodes/ 100 patients/year respectively (Figure). Once the treatment was established, the incidence of uveitis in patients with monoclonal antibodies TNFi became 9.4 episodes/ 100 patients/ year while in those treated with ETN and SECU was 24.2 and 50 episodes/100 patients/year respectively.
Conclusion: In our study, the prevalence of uveitis in patients with PsA was 4.9%. The pattern was similar to that observed in axSpA with acute onset and anterior and unilateral pattern. Patients who developed uveitis more frequently presented HLA-B27 positivity, sacroiliitis in MRI and ocular surface pathology, in addition to a higher PsAID score and the BASFI index. The uveitis rate decreased with the monoclonal antibodies TNFi, while an increase was recorded with ETN or SECU.
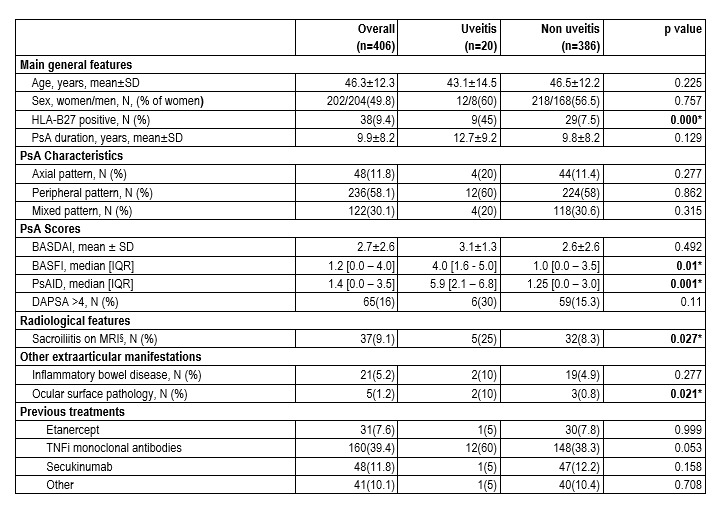 Table.General features of 406 patients with PsA. Comparison between patients with and without uveitis.
Table.General features of 406 patients with PsA. Comparison between patients with and without uveitis.
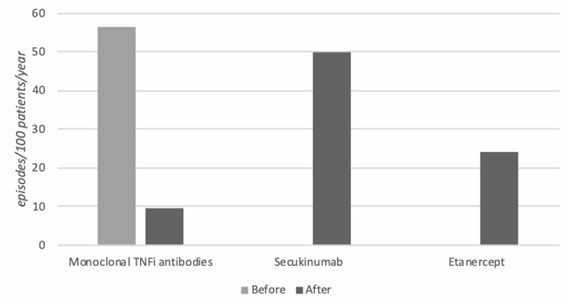 Figure. Uveitis incidence rate before and after biological therapy.
Figure. Uveitis incidence rate before and after biological therapy.
To cite this abstract in AMA style:
de Vicente Delmás A, Sánchez-Bilbao L, Calvo-Río V, Martinez-Lopez D, Herrero-Morant A, Galindez-Agirregoikoa E, Gonzalez-Mazon I, Barroso García N, PALMOU FONTANA N, Blanco R, gonzalez-Gay M. Uveitis in 406 Patients with Psoriatic Arthritis: Epidemiology, Clinical Characteristics and Relationship with Biological Treatment. Study of a Single University Center [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/uveitis-in-406-patients-with-psoriatic-arthritis-epidemiology-clinical-characteristics-and-relationship-with-biological-treatment-study-of-a-single-university-center/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uveitis-in-406-patients-with-psoriatic-arthritis-epidemiology-clinical-characteristics-and-relationship-with-biological-treatment-study-of-a-single-university-center/
