Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Uveitis is the most common extra-articular manifestation of axial spondyloarthritis (axSpA). It is characterized by sudden onset, acute, anterior and unilateral. The most widely used biological drugs for its treatment are TNF inhibitors (TNFi), especially monoclonal antibodies.
Our objectives were to evaluate a) epidemiological and clinical characteristics of patients with axSpA and uveitis, and b) the biological treatment received.
Methods: Cross-sectional study of patients with axSpA from a single referral hospital. They were diagnosed of axSpA according to the ASAS criteria. Demographic characteristics, clinical findings including extra-articular manifestations, and the treatment used were recorded. Those with ocular manifestations were evaluated by expert ophthalmologists for diagnosis and characterization of uveitis.
Results: We studied 301 patients with axSpA, 72.1% of them met New York criteria for Ankylosing Spondylitis (AS) and the remaining 27.9% met ASAS criteria for non-radiographic axSpA (nr-axSpA). 59.1% were male and the mean age was 52.16± 12.50 years. At the time of the study, 44 patients (14.6%) had developed at least one episode of uveitis (36 AS and 8 nr-axSpA). The uveitis pattern was anterior and acute (AAU) in all cases and 93% presented unilateral involvement.
The comparison of baseline characteristics between patients with axSpA with and without uveitis is shown in the Table. The group of patients with uveitis showed a higher delay in diagnosis (median [IQR]: 8.5[1-21] Vs 4[1-10], p=0.08) and a higher prevalence of HLA-B27 (84.1% Vs 59.5%, p=0.002).No differences were found in the other clinical characteristics collected (presence of peripheral arthritis, enthesitis and dactylitis throughout the disease, or BASDAI, BASFI or BASMI values at the time of the study). The presence of other extra-articular manifestations was also comparable in patients with and without AAU.
17 (38.6%) patients with AAU were treated with TNFi agents versus 115(44.7%) patients without AAU, with no differences between the diferents agents used. In both groups, the most widely used TNFi agents were Adalimumab, which received 13.6% and 22.6% (p=0.125) of patients with and without AAU, and Infliximab used in 13.6% and 10.9% (p=0.376) respectively. No differences were observed in the use of Etanercept.
Conclusion: In our series, 14.6% of the patients with axSpA had developed at least one episode of uveitis at the time of the study. Uveitis in patients with axSpA was anterior and acute in all cases and unilateral in 93%. Patients who developed AAU were characterized by a higher delay in diagosis and a higher prevalence of HLA-B27. No differences were found in the TNFi agents used in patients with and without AAU.
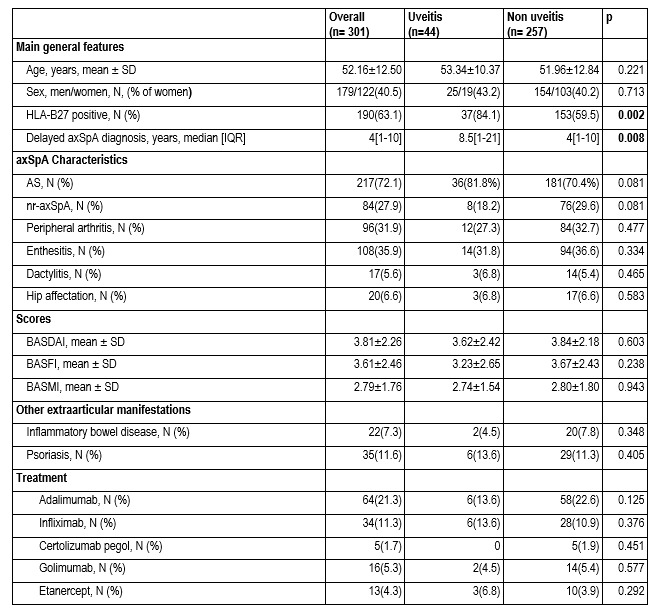 Table.General baseline characteristics of 301 patients with axSpA.Comparison between patients with and without uveitis.
Table.General baseline characteristics of 301 patients with axSpA.Comparison between patients with and without uveitis.
To cite this abstract in AMA style:
de Vicente Delmás A, Gonzalez-Mazon I, Rueda-Gotor J, Herrero-Morant A, Barroso García N, gonzalez-Gay M, Blanco R. Uveitis in 301 Patients with Axial Spondyloarthritis of a Single University Center: Epidemiology, Clinical Features and Biological Treatment [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/uveitis-in-301-patients-with-axial-spondyloarthritis-of-a-single-university-center-epidemiology-clinical-features-and-biological-treatment/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uveitis-in-301-patients-with-axial-spondyloarthritis-of-a-single-university-center-epidemiology-clinical-features-and-biological-treatment/
