Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
With rapid rise in healthcare costs, there is increased emphasis to teach cost-conscious care in graduate medical education. Our objective was to develop online cases to teach high-value care and diagnostic evaluation of musculoskeletal (MSK) complaints to pediatric residents and rotating medical students.
Methods:
Six online cases of common pediatric MSK complaints were developed utilizing a branched storyboard approach. Access and instructions on using the online modules were distributed during two scheduled lunchtime teaching conferences at University Hospitals Cleveland Medical Center.
Learners completed the modules in either one of two groups, those who saw the itemized costs of diagnostic tests and those who did not, to determine whether displaying costs would affect decision-making behavior and ability to arrive at a correct diagnosis. All learners completed a post-simulation survey. Measured outcomes included presumed diagnosis, cost of evaluation, diagnostic testing utilized, and perceptions towards the learning platform and high-value care. Simulation outcomes were assessed using paired t-tests. Survey data between the two groups was analyzed with Chi-squared tests. Outcomes separated by training year was analyzed using ANOVA and a post-hoc Tukey test.
Results:
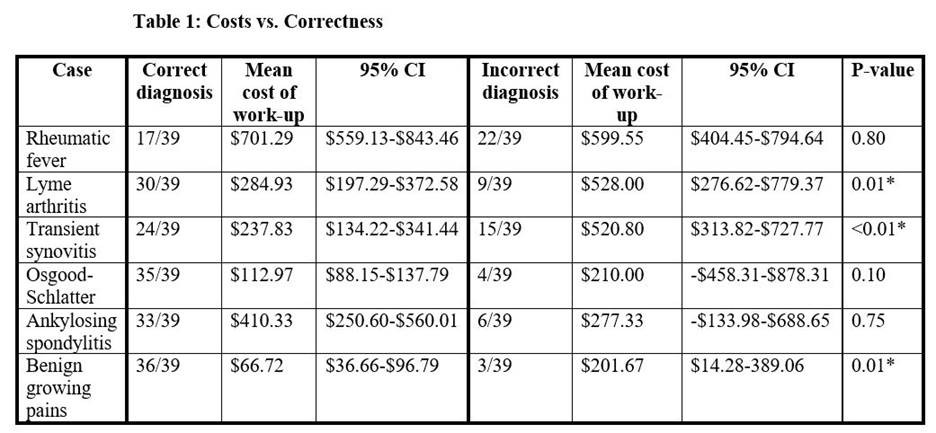
A total of 39 residents and medical students participated in the pilot and completed the survey. Learners were randomly assigned to complete the simulated cases with costs (n=19) or no costs (n=20) displayed next to orderable tests during the diagnostic workup. Overall, learners who were able to see costs of diagnosis spent less money on diagnostics ($1511.11 mean per learner versus $2311.35, p = 0.01). Arrival at the correct diagnosis was associated with lower costs in 3 of 6 cases (Table 1). When compared to the no cost group, learners in the group that had access to costs reported feeling more knowledgeable about the price of diagnostic tests post-simulation (p=0.04) and were more likely to factor costs into their practice moving forward (p=0.03). Third year residents demonstrated a statistically significant increase in number of cases diagnosed correctly as opposed to medical students.
Conclusion:
Our data showed that those who made incorrect diagnoses often spent more money, stressing the need for proper clinical training to prevent wasted healthcare costs. Overall, learners expressed preference for using online cases as a learning tool and recognized high-value care as an important component of patient care after completion of the simulation. This suggests that simple interventions that challenge learners to integrate costs into decision-making can be the basis for changing future practice.
To cite this abstract in AMA style:
Yip A, Morris S, Buchner M, Robinson A. Using Online Simulation of Pediatric Musculoskeletal Cases to Evaluate How Knowledge of Costs Affects Diagnostic Workup [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/using-online-simulation-of-pediatric-musculoskeletal-cases-to-evaluate-how-knowledge-of-costs-affects-diagnostic-workup/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-online-simulation-of-pediatric-musculoskeletal-cases-to-evaluate-how-knowledge-of-costs-affects-diagnostic-workup/