Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Fibrotic lung diseases encompass a wide spectrum of clinical entities including connective tissue disease related interstitial lung disease (CTD-ILD) and interstitial pneumonia with autoimmune features (IPAF). Prior research on serum Krebs von den Lungen-6 (KL-6), surfactant proteins A (SP-A) and D (SP-D) levels have shown independent correlation to disease severity in patients with CTD-ILD. To our knowledge, no studies have evaluated the utility of all three biomarkers in predicting disease severity among US patients with CTD-ILD/IPAF. The goal of this study is to assess 1) the correlation between these biomarkers and lung disease severity; 2) their combined use with forced volume capacity (FVC, % predicted) in predicting lung disease severity using high resolution computed tomography (HRCT) as reference for disease severity.
Methods: This retrospective cross-sectional study involves 20 patients who had testing performed for ILD autoantibodies and KL-6, SP-A, and SP-D biomarkers at ARUP laboratories. In addition, they were diagnosed with CTD-ILD/IPAF per ACR criteria and had HRCT and pulmonary function testing available within 3 months from the date of the laboratory assessments. Positive KL-6, SP-A and SP-D levels were defined as >500 U/mL, >200 ng/mL and >300 ng/mL respectively. Extent of pulmonary fibrosis on HRCT was estimated as 0 to 100 percent using the Athol-Wells method. We evaluated correlations between each biomarker and disease severity and assessed the individual and combination weights of KL-6, SP-A and SP-D levels and FVC in predicting disease severity (dependent variable) using HRCT as reference for disease severity.
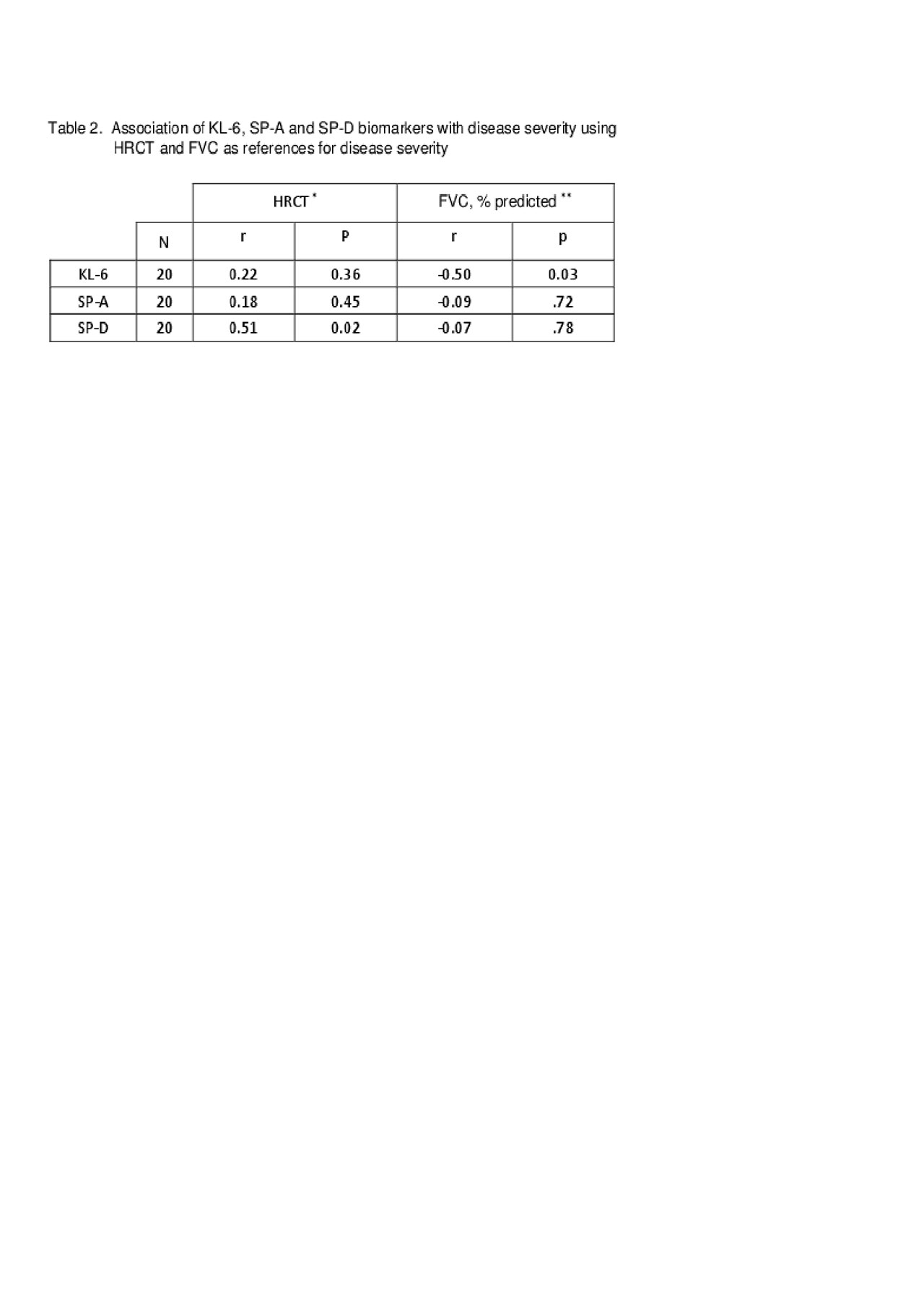
Results: 75% of patients were white and 65% were females. 75, 25 and 75% had positive KL-6, SP-A and SP-D levels respectively (Table 1). All three biomarkers had positive correlations with disease severity, but only SP-D level had significant correlation with disease severity (r = 0.51, p: 0.02) (Table 2). KL-6 levels had significant negative correlation with FVC (r = 0.50, p: 0.03), but not with HRCT. In addition, SP-A levels were elevated in patients with severe disease as compared to those without (p: 0.03) (Table 3). In univariate regression analyses of KL-6, SP-A, SP-D and FVC only SP-D level had significant correlation in predicting disease severity (r = 0.05, p: 0.02) whereas in a multiple regression model using KL6, SPA, SPD, and FVC as independent variables, SPD (r = 0.08, p: 0.006) and FVC (r = – 0.74, p: 0.03) were found to have statistically significant coefficients. Thus, all other predictor variables being equal, a one unit increase in SP-D is associated on average with a 0.064 increase in disease activity (R2: .47, F-Value: 0.03).
Conclusion: The findings in this single-center retrospective study of patients with CTD-ILD/IPAF suggest that use of lung injury specific biomarkers and FVC together may be valuable in predicting disease severity and offer a cost-effective approach in monitoring disease progress. To our knowledge, this is the first US cohort study evaluating the utility of all three biomarkers in predicting disease severity among patients with CTD-ILD/IPAF.
** ILD autoantibodies includes: ANA, RF, CCP, Jo-1, EJ, OJ, PL-7, PL-12, SRP, SCL-70, centromere, RNAP III, U1RNP, PM/SCL-100, Ku, SSA-52, and SSA-60. Testing performed at ARUP Inc.
*Quantitative high resolution CT score used to determine disease severity
**Forced vital capacity used to determine disease severity
To cite this abstract in AMA style:
Amjadi S, Frech T, Chan J, Scholand M, Jaskowski T, La’ulu S, Genzen J, Lebiedz-Odrobina D, Tebo A. Use of Serum Lung Injury Biomarkers for Predicting the Severity of Interstitial Lung Disease in Patients with Connective Tissue Disease Associated Interstitial Lung Disease and Interstitial Pneumonia with Autoimmune Features [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/use-of-serum-lung-injury-biomarkers-for-predicting-the-severity-of-interstitial-lung-disease-in-patients-with-connective-tissue-disease-associated-interstitial-lung-disease-and-interstitial-pneumonia/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-serum-lung-injury-biomarkers-for-predicting-the-severity-of-interstitial-lung-disease-in-patients-with-connective-tissue-disease-associated-interstitial-lung-disease-and-interstitial-pneumonia/