Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The increase in therapeutic options for our Pediatric Rheumatology patients has led to improved outcomes but has increased the number of immunocompromised (IC) patients. A reliable method of identifying IC patients is essential to their care. However, there is currently no automated method in our electronic medical record (EMR) that identifies a patient as IC. Relying on physician or staff identification of IC has the potential for human error and/or oversight, is time consuming and has not been standardized. The aim of our study was to formulate an IC operational definition to be used in an automated report via our EMR to accurately identify patients who should be classified as IC based on their current diagnoses and/or medications.
Methods: An operational definition of IC status was constructed and included 173 ICD-10 diagnostic codes and 617 immunosuppressant medications. These parameters were assembled in an EMR grouper-based report that was able to filter and flag IC patients scheduled in our clinic. Our EMR report’s performance was tracked by comparing its identification accuracy to a pediatric rheumatologist and nurse evaluation. Daily reports for five consecutive weeks were screened including a total of 448 patients scheduled. These comparisons were tracked and adjustments were made to operational definition based on EMR failures.
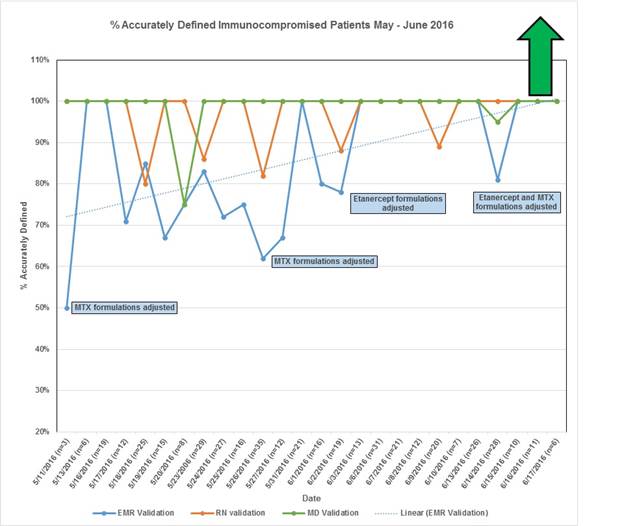
Results: In total, 214 patients were found to be IC during our data collection, based on multi-provider consensus. The physician and nurse continued to produce instances of human screening error, but our EMR performance steadily improved during our period of analysis. (Chart 1) The most common reason for our EMR failure to capture patients was formulation variations in our commonly utilized medications. Taking into account its cumulative improvement overtime, our EMR was able to capture 84% of the IC patients. The accuracy of the EMR is anticipated to reach 100% as we are able to obtain a complete list of all the names used for Methotrexate and Etanercept.
Conclusion: We have demonstrated that using EMR to identify IC patients is a unique and effective method that will provide level of reliability 3 (LOR#3). Automated identification of IC patients in Pediatric Rheumatology is efficient and will ultimately lead to better outcomes for our complex patient population. We believe that our EMR process of identifying IC patients is transferrable to other subspecialties and centers caring for similar at-risk patients. Once the operational definition for the EMR is perfected, we will use the EMR identification of IC to generate an automated report of Hepatitis B and Pneumococcal serologies, vaccination data, as well as Tuberculosis screening. In addition, we will be able to automatically notify other healthcare providers of IC status that will assist with potential harmful exposures such as live virus vaccines.
To cite this abstract in AMA style:
Favier LA, Smitherman EA, Furnier A, Ting T, Watts A, Kramer S, Parwani M, Huggins JL. Use of Electronic Medical Record to Identify Immunocompromised Patients in a Pediatric Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/use-of-electronic-medical-record-to-identify-immunocompromised-patients-in-a-pediatric-rheumatology-clinic/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-electronic-medical-record-to-identify-immunocompromised-patients-in-a-pediatric-rheumatology-clinic/