Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Facing fixed time for specialty visits, the time staff spends on rooming patients is a premium, but remains poorly understood. We conducted a time study, a basic systems engineering approach, to examine the frequency and duration of all visit related tasks performed by clinic staff (medical assistants (MA) or nurses) between the waiting room and the entry of the rheumatologist.
Methods: We developed a time study tool using health system policies and procedure documents, interviews and observations of pre-visit rooming. The tool measured 25 pre-determined tasks at a resolution of 15s=0.25 min. Trained engineering and medical observers measured 190 rooming sequences for a total of 1419 minutes at three rheumatology clinics in an academic multispecialty practice during Fall 2014-Spring 2015. Rooming was performed by nurses or MA at 2 sites, but otherwise by MAs. Scheduled visits varied from 20-30 minutes. We calculated descriptive statistics on tasks and times, compared frequencies using Fischer’s exact test, and times using analysis of variance. We developed a task taxonomy and described variations in tasks.
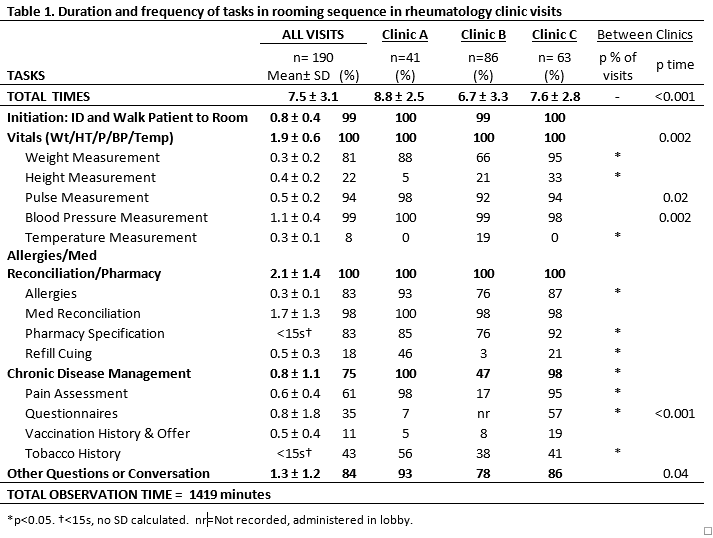
Results: We observed 18 additional actions beyond 25 expected tasks. We then grouped 15 labeled tasks in 5 categories based on the sequence they occurred and clinical objectives for each task (Table 1). Total rooming time varied widely (2.5-22 min). Mean rooming time was 7.5 ± 3.1 min across clinics (Table 1) and varied between clinics, at 8.8, 6.7, and 7.6 minutes (p<0.001).
Vital signs (1.9 ± 0.6 min) and medication reconciliation (1.7 ± 1.3 min) accounted for half of the total rooming time. Maximum time variation was associated with questionnaire administration (±1.8 min), medication reconciliation (±1.3 min), and other conversations (± 1.2 min). Only 4 tasks were observed in >90% of the rooming sequences: initiation, pulse, blood pressure measurement, and medication reconciliation. For other tasks, frequencies varied by clinic. For instance, prescription refills occurred in 3 vs. 46% of clinic visits, and pain scores in 17 vs. 98% of visits when stratified by clinic (p=<0.001). Five of nine tasks with high frequency variation were identified to benefit from standardization: height, weight measurement, prescription refill cueing, pain assessment, questionnaire administration (disease activity, new patient) and tobacco history.
Conclusion: Using time study we developed a practical tool for measuring time spent on each rooming task, and created a taxonomy of rooming tasks. We found that the frequency and timing of rooming tasks varied among encounters and clinics. Implications of this work beyond our institution include methods for (A) identifying and prioritizing opportunities for standardization, (B) offering a platform for decisions regarding changing standards and (C) comparing baseline data for new scheduling or care quality initiatives.
To cite this abstract in AMA style:
Stroik B, Bartels CM, Lauver D, McBride P, Arnason J, Loring S, Ramly E. Unwanted Variations in Rheumatology Clinic Rooming: A Time Study Tool and Analysis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/unwanted-variations-in-rheumatology-clinic-rooming-a-time-study-tool-and-analysis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/unwanted-variations-in-rheumatology-clinic-rooming-a-time-study-tool-and-analysis/