Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Mental health disorders are prevalent in patients with rheumatic diseases, particularly since many of these diseases present early, have a chronic course, and significantly impact one’s daily function. The prevalence of depression and anxiety in SLE is 71-80%.2 Depression in RA is up to 50%.1 Some medications (i.e. steroids) also bear potential mental health effects. Rheumatology patients with psychiatric comorbidities use healthcare resources more than their counterparts. While rheumatologists demonstrate awareness of mental health disorders in their patients, utilization of formal screening tools and mental health services is lacking.
Methods: We evaluated all patients referred from the rheumatology clinic at a tertiary care center to mental health providers (psychiatry/psychology/neuropsychology) over a 2-year period (2/2019 – 2/2021). Data collected included age, sex, underlying rheumatic disease, additional medical and psychiatric comorbidities, and reason(s) for referral to mental health services. Subsequent appointments with a mental health provider were noted.
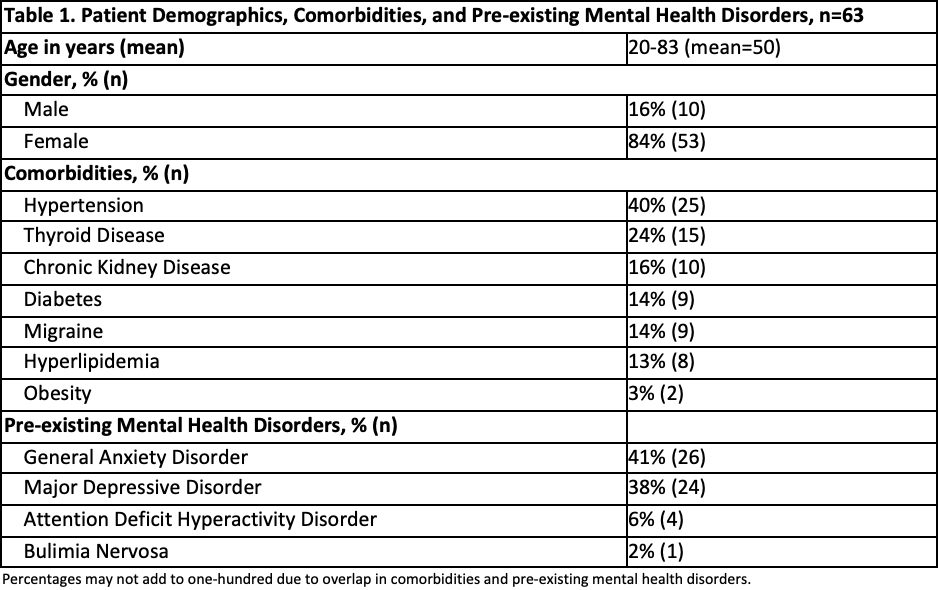
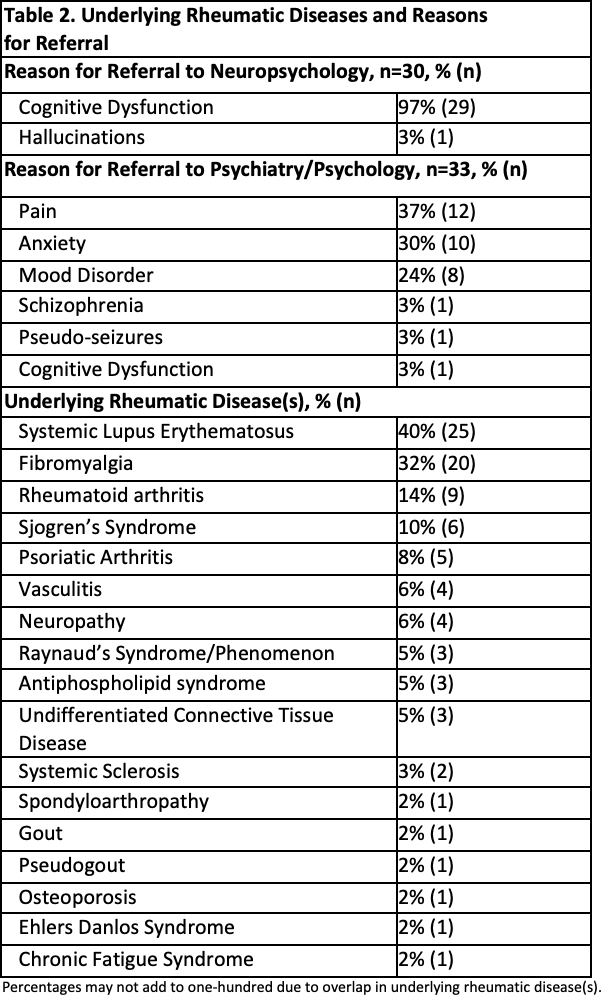
Results: Of 6154 patients seen in the rheumatology clinic over 2 years, only 63 (1%) were referred to mental health providers. Patient demographics and underlying comorbidities are noted in Table 1. The age range of patients was 20-83 years, of whom 84% were female. Reasons for referral are noted in Table 2. 48% of referrals were for neuropsychology, most commonly for evaluation of cognitive dysfunction. 52% of referrals were for psychiatry/psychology, most commonly for evaluation of chronic pain, anxiety, and mood disorders. While most patients had multiple rheumatic diagnoses, SLE was the most common underlying rheumatic disease diagnosis in patients who were referred to mental health (40%), followed by fibromyalgia (32%) and RA (14%). Only 1/3rd of patients originally referred for mental health services were seen by a mental health provider.
Conclusion: Our findings demonstrate a significant underutilization of mental health services by rheumatologists. This is particularly worrisome since our institutional behavioral health and neuropsychology departments offer comprehensive treatment for a variety of mental and behavioral health issues. Although we recognize that the COVID-19 pandemic and limitations of telehealth visits may have contributed to the lower referrals to mental health services, there was, in fact, a greater need for mental health optimization during this time, with anxiety and depression being more prevalent in patients with rheumatic disease during the COVID-19 pandemic. Our study serves as a call for action to appropriately assess and timely refer patients to mental health providers. Further studies on reasons for lack of follow up may provide additional insight for improvement in the care of these patients
References:
1. Lwin MN et al. Rheumatoid Arthritis: The Impact of Mental Health on Disease: A Narrative Review. Rheumatol Ther. 2020 Sep;7(3):457-471
2. Moustafa AT et al. Prevalence and metric of depression and anxiety in systemic lupus erythematosus: A systematic review and meta-analysis. Semin Arthritis Rheum. 2020 Feb;50(1):84-94.
To cite this abstract in AMA style:
Lim D, Aggarwal M, Sandhu V. Underutilization of Mental Health Services in a Busy Tertiary Care Rheumatology Facility [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/underutilization-of-mental-health-services-in-a-busy-tertiary-care-rheumatology-facility/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/underutilization-of-mental-health-services-in-a-busy-tertiary-care-rheumatology-facility/