Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Sarcoidosis is an inflammatory disorder of unknown etiology characterized by tissue infiltration with non-caseating granulomas which can affect any organ. The most common organ involved is the lungs but involvement of eyes (Uveitis), skin (Cutaneous), lymph nodes, gastrointestinal (GI), upper respiratory tract (URT), musculoskeletal system (Arthritis), heart and central nervous system can be seen as well. Systemic glucocorticoid therapy has been proven to improve and stabilize pulmonary and extrapulmonary Sarcoidosis but are associated with a plethora of undesirable side effects. There is a paucity of guidelines and clinical trial data are limited for the steroid sparing agents to treat chronic Sarcoidosis, so majority of the treatment decisions are based solely on extrapolation from studies done for other autoimmune diseases and expert opinion. This study aims to review the various organ manifestations and treatment options used to successfully treat patients of Sarcoidosis at our academic center.
Methods: This is a retrospective chart review of 172 patients seen in our rheumatology clinic with the diagnosis of Sarcoidosis. Categorical analysis was performed by Chi-squared analysis unless the underlying assumptions were violated when Fisher’s exact test was used instead. Continuous measures, such as age, were compared between groups by a Student’s t test. P value of < 0.05 was considered significant.
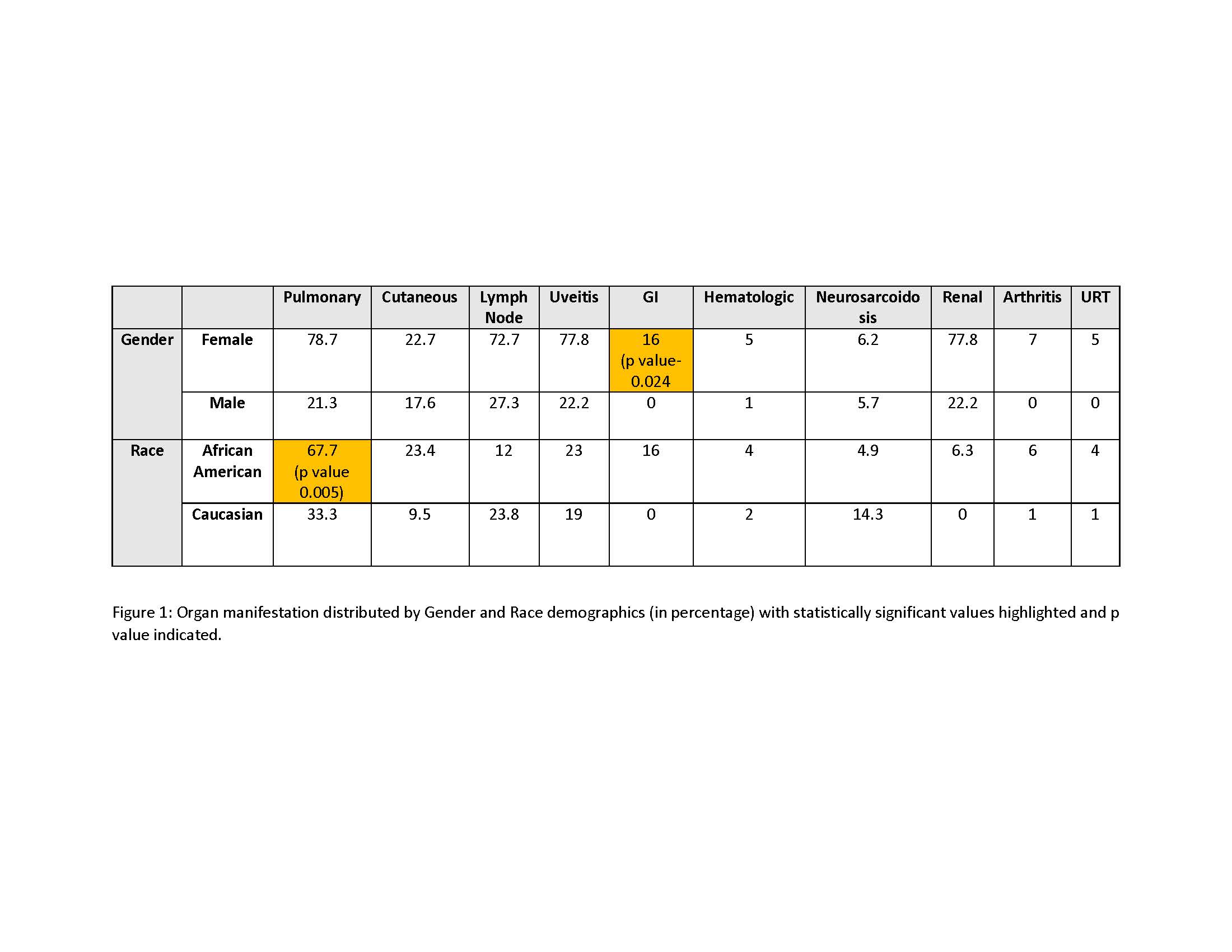
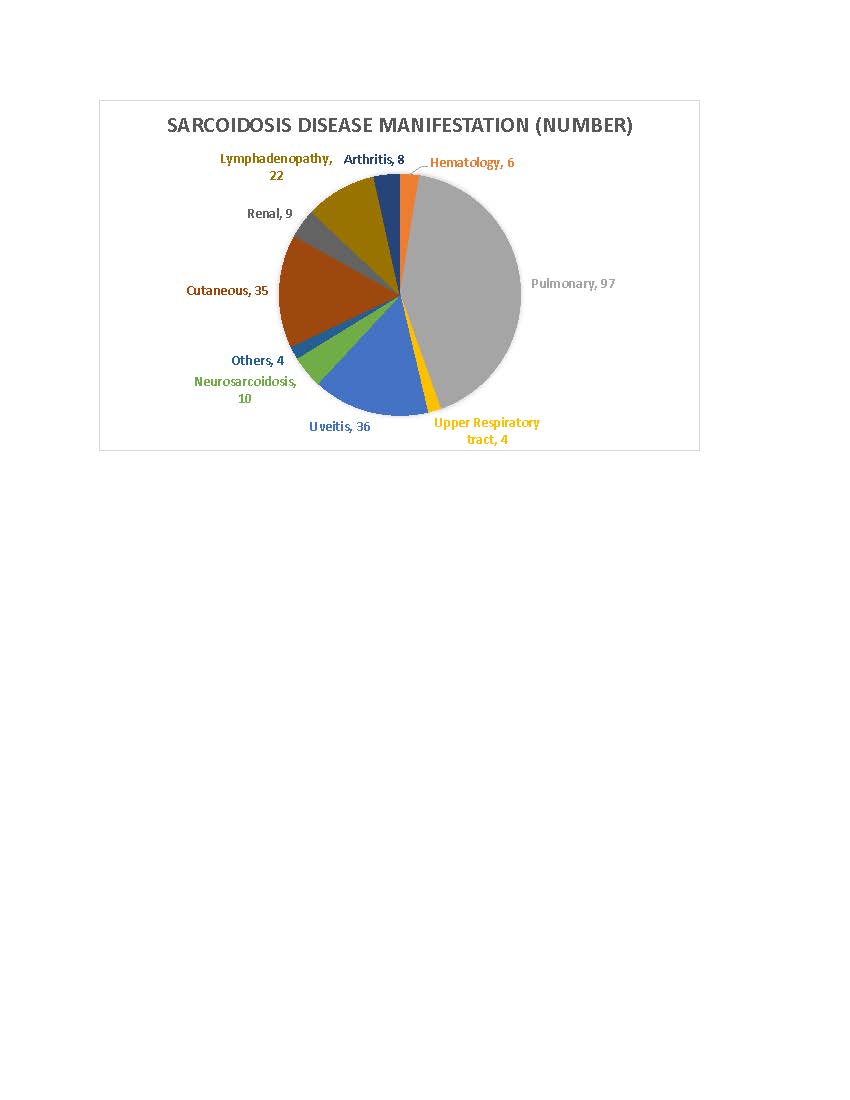
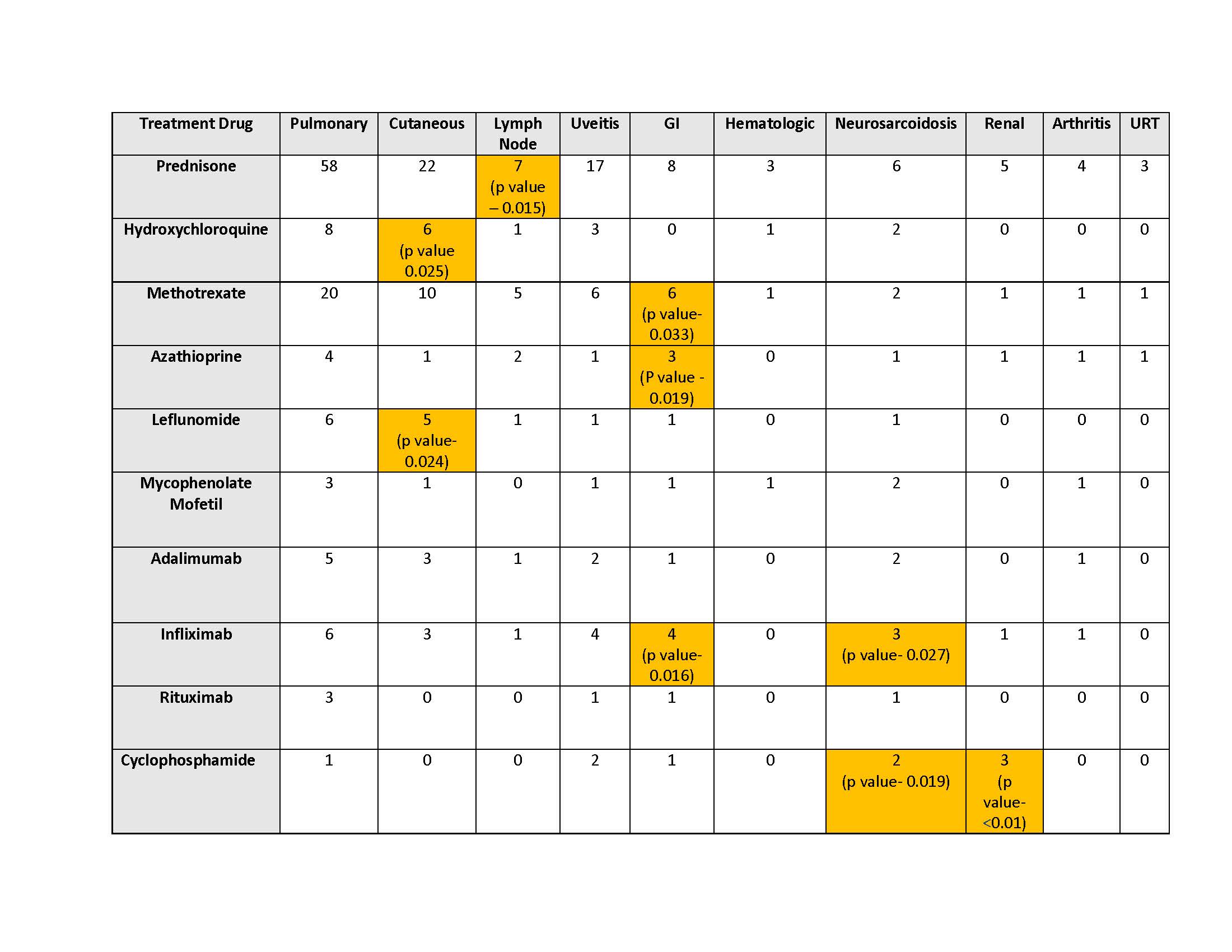
Results: Sarcoidosis was seen to affect patients between the age of 17 – 83 years (Mean 49.3). Females diagnosed with Sarcoidosis were older than males (p value 0.006). There was no association found between the age, gender and race except that Pulmonary Sarcoidosis was significantly associated with African American population (p value 0.005) and GI involvement was seen in females (p value 0.024) (Fig. 1). The most common organ manifestations were Pulmonary Sarcoidosis seen in 97 patients (56.4%), Uveitis in 36 patients (20.9%) and cutaneous Sarcoidosis in 35 patients (20.3%) (Fig 2). 81 patients (46.8%) had more than one organ involvement. Amongst the treatment agent for each organ manifestations, statistically significant associations were found with Prednisone for Lymph node involvement (p value 0.015); Hydroxychloroquine for Cutaneous Sarcoidosis (p value 0.025); Methotrexate (p value 0.033), Azathioprine (p value 0.019) and Infliximab (p value 0.016) for GI involvement; Infliximab (p value 0.027) and Cyclophosphamide (p value 0.019) for Neurosarcoidosis; and Cyclophosphamide for renal involvement (p value < 0.01). The Prednisone dose was variable between 5 mg to 60 mg with a mean of 15 mg.
Conclusion: The most common manifestation was noted to be Pulmonary involvement followed by Uveitis and cutaneous Sarcoidosis and Pulmonary Sarcoidosis was more common in African Americans. The prescribing practice at our center for chronic Sarcoidosis with statistical significance included Hydroxychloroquine for Cutaneous; Methotrexate and Azathioprine for GI involvement, Infliximab for GI and Neurosarcoidosis. Long term prospective studies need to be done to outline a treatment protocol for patients with chronic Sarcoidosis to limit the use of long term steroids.
To cite this abstract in AMA style:
Tariq M, Katikaneni M, Malhotra K, McLarty J, Umer S, Hayat S. Understanding the Mystery of Sarcoidosis: An Academic Rheumatology Center Experience [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/understanding-the-mystery-of-sarcoidosis-an-academic-rheumatology-center-experience/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-the-mystery-of-sarcoidosis-an-academic-rheumatology-center-experience/