Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: The COVID-19 pandemic has caused great concern amongst immunocompromised patients, especially those with rheumatic diagnoses. While much has been learned in the past two years about populations at risk for severe disease and the need to suppress the hyperinflammatory response from COVID-19 infection, still much is uncertain about outcomes related to the underlying rheumatic conditions and the medications used to treat these conditions. The aim of this project is to investigate underlying risk for severe outcomes following infection with COVID-19, including stratification across rheumatic diagnosis, comorbidities, and medications.
Methods: We performed a retrospective cohort study in patients with rheumatic diseases who tested positive for COVID-19 and were being followed by the VCU Rheumatology Clinic between March 01, 2020 – May 31, 2021. Data analysis was performed using a Chi-square test and relative risk estimate. We categorized severe COVID-19 outcomes as: admission, supplemental oxygen, ICU care, intubation, and death. Age, sex, rheumatic disease diagnosis, comorbidities, and rheumatic disease medications taken prior to infection were analyzed as potential risk factors for severe COVID-19 outcomes.
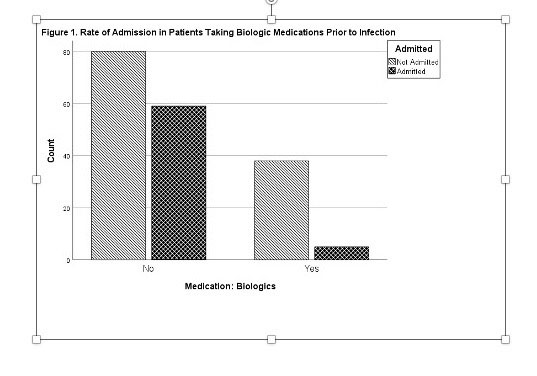
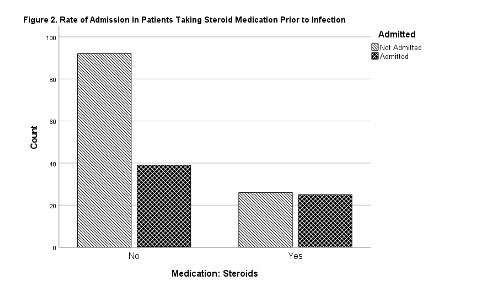
Results: We identified 182 cases of patients who met the above criteria. Of these cases, 64 (35.2%) were admitted due to COVID-19 infection, 35 (19.2%) required supplemental oxygen, 14 (7.7%) required ICU care, and 5 (2.7%) died. In a relative risk analysis, patients who were >65 years of age (RR 2.53, 95% CI 1.80-3.57) and used steroids (RR 1.647, 95% CI 1.12-2.42) were both associated with an increased risk of hospitalization. Use of biologics prior to infection was associated with a lower risk of hospitalization (RR 0.274, 95% CI 0.12-0.64) and were less likely to need supplemental oxygen (RR 0.3, 95% CI 0.098-0.941). No relation was seen between rheumatic disease diagnosis and severity of COVID-19 outcome. An increased risk of hospitalization was associated with certain comorbidities, including CAD (RR 1.9, 95% CI 1.16-3.13), COPD (RR 1.99, 95% CI 1.2 -3.3), kidney disease (RR 1.87, 95% CI 1.23-2.85), and diabetes (RR 1.75, 95% CI 1.19-2.56).
Conclusion: Based on our data, a patient’s rheumatic diagnosis is not an independent risk factor for hospitalization and ICU admission from COVID-19 infection. Patients taking biologic agents were at decreased risk for hospitalization. However, patients on chronic steroids were at increased risk for hospitalization for COVID-19 infection.
To cite this abstract in AMA style:
Allcott N, Gupta N, Raghavan N, Syed H, Danielides S. Uncovering the Relationship Between COVID-19 Outcome Severity and Rheumatic Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/uncovering-the-relationship-between-covid-19-outcome-severity-and-rheumatic-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uncovering-the-relationship-between-covid-19-outcome-severity-and-rheumatic-disease/