Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Ultrasound (US), magnetic resonance imaging (MRI) and conventional radiography are the leading imaging modalities for musculoskeletal (MSK) assessment in PsA. However, little is reported about the discrepancies between these tools in PsA patients. The aim of this study is to examine the agreement between these modalities and to evaluate the sensitivity and specificity of US and X-ray with MRI as gold standard in PsA patients.
Methods: The study population included consecutive PsA patients (CASPAR criteria) that were prospectively recruited. All patients underwent clinical assessment including complete history taking, physical examination, questionnaires for disease activity and quality of life assessment and blood test for acute phase reactants. US (gray scale and Doppler), contrast enhanced MRI and AP and oblique radiographs of MCP, PIP and DIP joints of one most clinically involved matched hand. US and MRI evaluated synovitis, flexor tenosynovitis and extensor paratenonitis. US, MRI and radiography evaluated erosions and bone proliferations. The time interval between the US and MRI was maximum 3 days and the US, MRI and X-ray readers were blinded to clinical data. NSAIDs were hold for 3 days before US and MRI assessment. The US images were scored according to the EULAR-OMERACT, the MRI images according to the PsAMRIS scoring system and the X-ray according to the Psoriatic Arthritis Ratingen Score (PARS) method. Positive values for comparison were ≥1. Agreement between MRI and US was calculated based on kappa and prevalence-adjusted bias-adjusted kappa (PABAK) values. Sensitivity and specificity of US and X-ray with MRI as gold standard was calculated as well.
Results: One hundred PsA patients were included (mean age: 51.2 years with 59% females) and 29 patients were in minimal disease activity. The prevalence of synovitis, flexor tenosynovitis, extensor paratenonitis were similar between the US and MRI assessments. Erosions were significantly increased in US and MRI compared to X-RAY in MCPs level (p=0.005), while bone proliferations were significantly increased in US and X-ray compared to MRI (p< 0.001) (Table 1). The absolute agreement between US and MRI was good-very good for synovitis (85%-96%, PABAK=0.7-0.92), flexor tenosynovitis (93%-98% PABAK=0.87-0.96) and for extensor paratenonitis (95%-98%, PABAK=0.9-0.97) (Table 2). Agreement between US, MRI and X-Ray for erosions was very good (96%-98%, PABAK=0.92-0.97) and for bone proliferations good-very good (71%-93%, PABAK= 0.47-0.87). Sensitivity of US with MRI as gold standard was higher for synovitis 0.5-0.86, extensor paratenonitis (0.63-0.85) than for flexor tenosynovitis (0.1-0.75), while the specificity was high in each evaluated domain (0.89-0.98) (Table 3).
Conclusion: There is very good agreement between US and MRI for the detection of finger inflammatory changes. US, X-ray and MRI have good to very good agreement for structural changes.
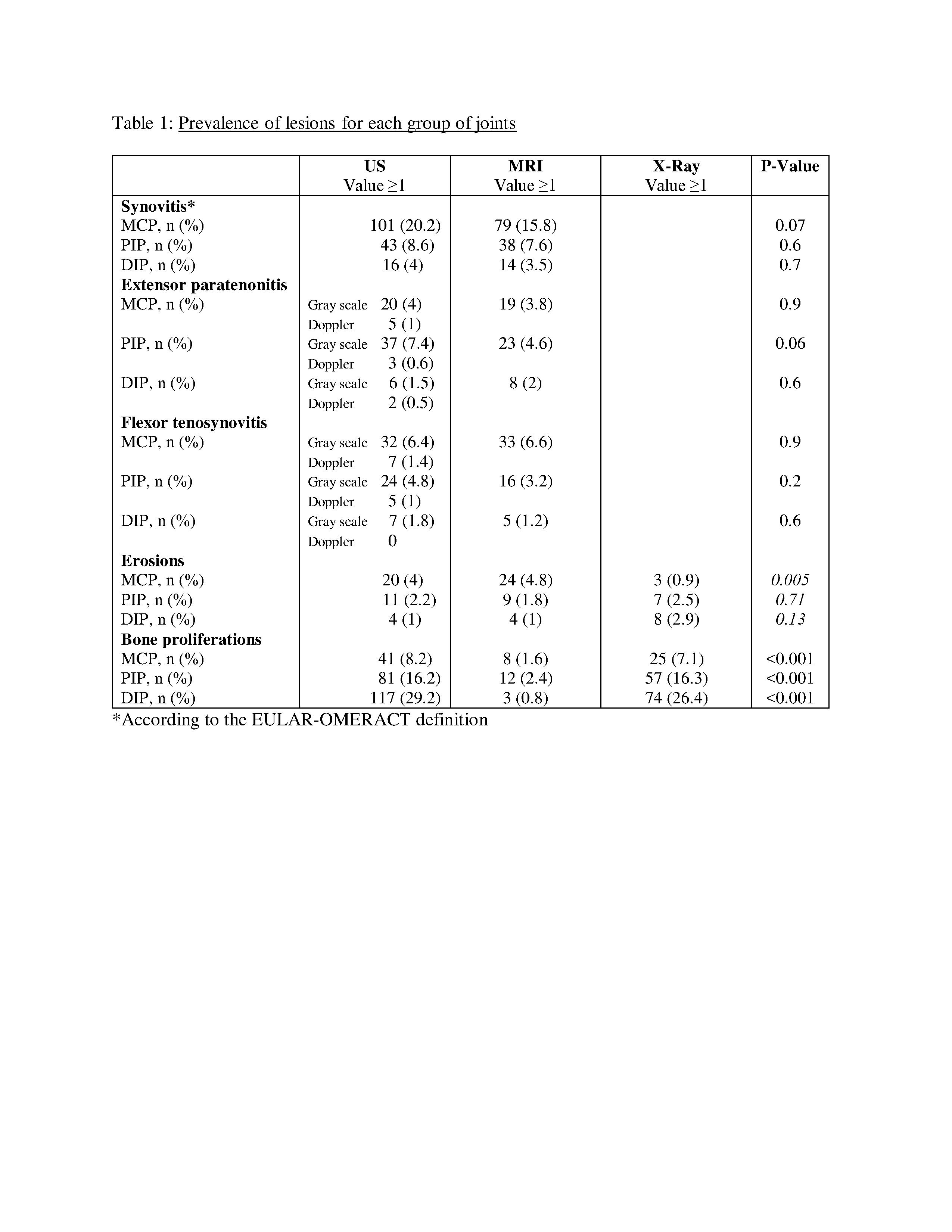 Table 1: Prevalence of lesions for each group of joints
Table 1: Prevalence of lesions for each group of joints
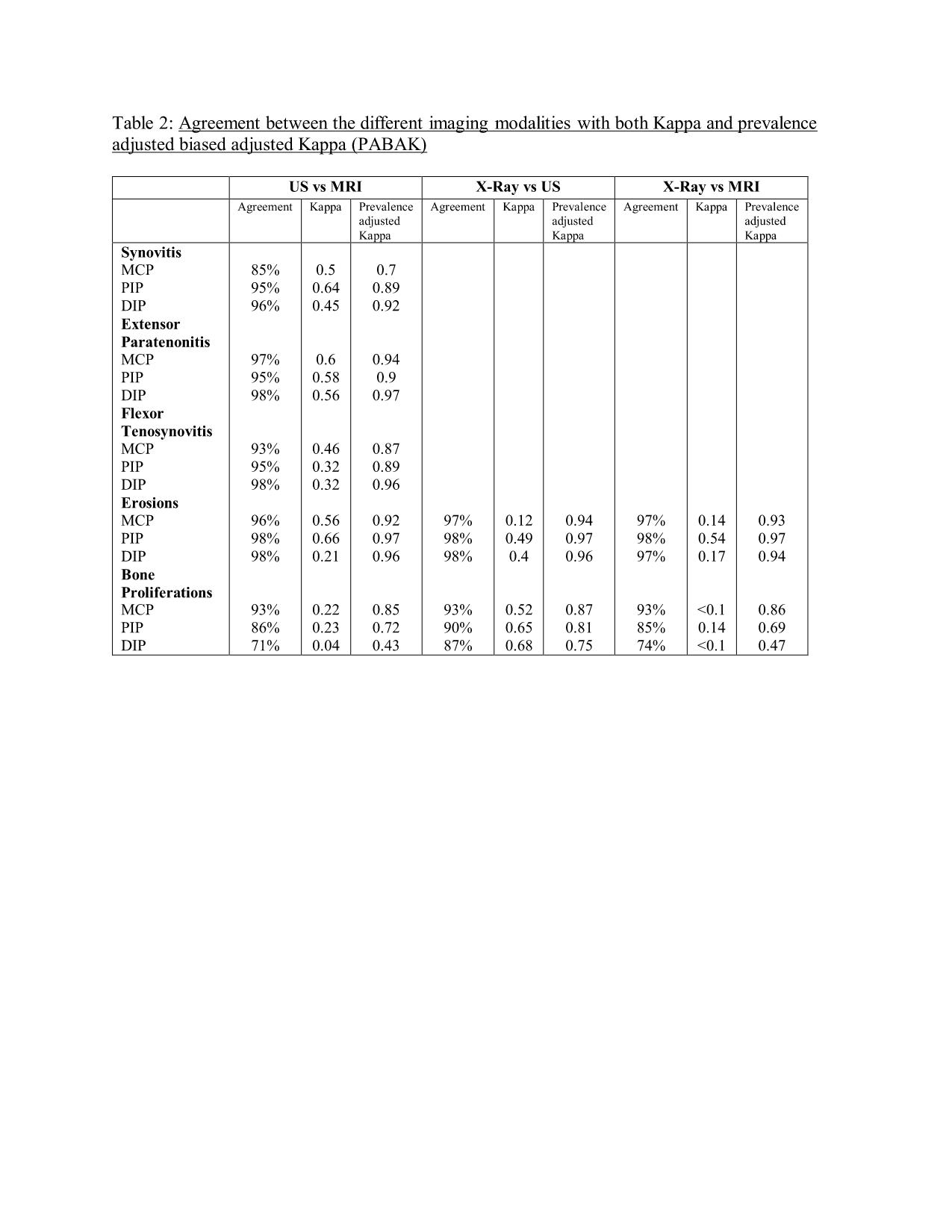 Table 2: Agreement between the different imaging modalities with both Kappa and prevalence adjusted biased adjusted Kappa (PABAK)
Table 2: Agreement between the different imaging modalities with both Kappa and prevalence adjusted biased adjusted Kappa (PABAK)
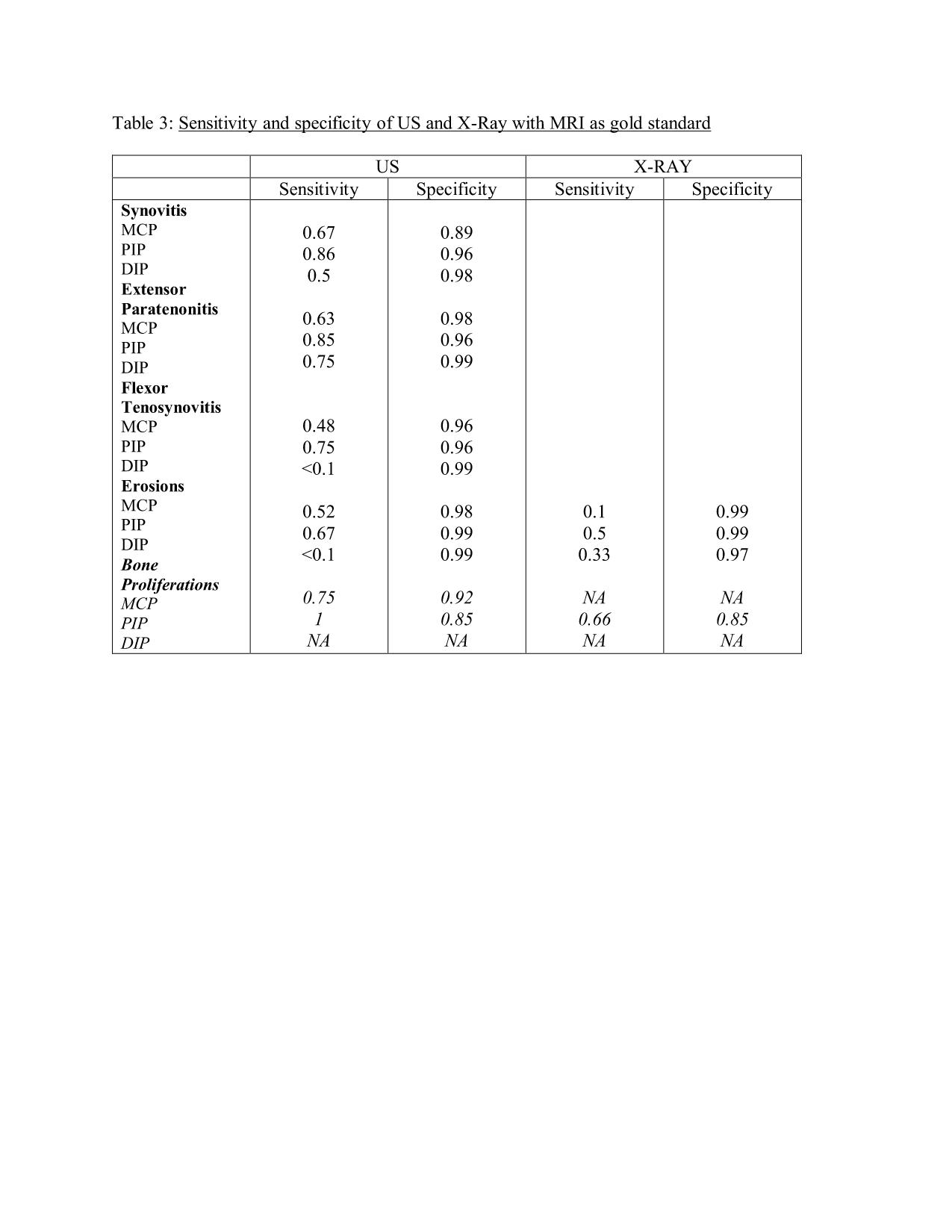 Table 3: Sensitivity and specificity of US and X-Ray with MRI as gold standard
Table 3: Sensitivity and specificity of US and X-Ray with MRI as gold standard
To cite this abstract in AMA style:
Polachek A, Furer V, Zureik M, Nevo S, Mendel L, Levartovsky D, Wollman J, Aloush V, Tzemach R, Elalouf O, Anouk M, Berman M, Kaufman I, Lahat goldstein Y, Sarbagil-Maman H, Borok Lev-Ran S, Broide A, Eder L, Paran D, Iluz M, Eshed I, Elkayam O. Ultrasound, Magnetic Resonance Imaging and Radiography of the Fingers’ Joints of Psoriatic Arthritis Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/ultrasound-magnetic-resonance-imaging-and-radiography-of-the-fingers-joints-of-psoriatic-arthritis-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ultrasound-magnetic-resonance-imaging-and-radiography-of-the-fingers-joints-of-psoriatic-arthritis-patients/
