Session Information
Date: Sunday, November 17, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Fast-track clinics utilizing ultrasound in the initial evaluation of patients with suspected giant cell arteritis (GCA) have been implemented throughout Europe allowing for rapid evaluation, a reduced incidence of vision loss and overall cost savings. Ultrasound is established as the recommended initial diagnostic modality for GCA in Europe, assuming availability and expertise per EULAR guidelines, and is now acknowledged as an alternative to temporal artery biopsy in the United States per the most recent ACR/EULAR classification criteria for GCA. In the United States, the use of ultrasound for GCA diagnosis has been limited to date. Here we report our point-of-care ultrasound fast-track GCA clinic experience at Massachusetts General Hospital.
Methods: A fast-track GCA clinic was developed at our tertiary care academic medical center which serves as a referral center for GCA patients. A standardized algorithm was created for referred patients with suspected GCA. Clinical evaluation and a dedicated color doppler ultrasound exam of the bilateral temporal and axillary arteries were completed in a single clinic session within 72 hours of referral as able. The bilateral temporal arteries (common superficial, parietal, and frontal branches) and bilateral axillary arteries were evaluated for hypoechoic vessel wall thickening (halo sign) according to established cutoff values. A 22 MHz ultrasound probe was used for temporal artery evaluation and a 12-15 MHz probe for axillary artery. Clinical evaluation and ultrasound exam were performed and interpreted by one rheumatologist (MAM). The first 50 ultrasound exams and then subsequent questionable ultrasound images were reviewed separately by a blinded rheumatologist (MJK), both with expertise in vasculitis ultrasound.
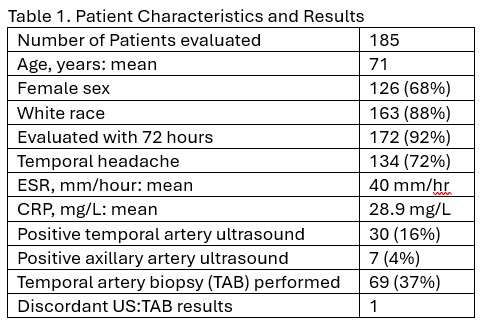
Results: Between September 2019 and mid-June 2024, 185 patients were evaluated in the fast-track GCA clinic. Overall, 172 patients (92%) were seen within 72 hours, mean age was 71 years, 68% were female and 88% were Caucasian. Temporal headache was reported by 72% of patients. Mean ESR was 40 mm/h and mean CRP was 28.9 mg/L. 37 patients (20%) had a positive temporal (n = 30) or axillary (n = 7) artery ultrasound. In total, 69 patients (37%) underwent TAB. There was 1 discordant result between ultrasound and TAB in a patient with a positive ultrasound and a biopsy that showed prominent Monckeberg sclerosis (Table 1). Twenty-two patients with negative results on both ultrasound and TAB went on to be treated for GCA given clinical suspicion. No patients developed vision loss attributed to GCA after evaluation.
Conclusion: Ultrasound at the point-of-care is an effective diagnostic tool in GCA, assuming adequate training and availability. For a subset of patients with negative ultrasound and TAB, the diagnosis of GCA can be made clinically.
References:
1) Ponte C et al, DCVAS Study Group. 2022 American College of Rheumatology/EULAR classification criteria for giant cell arteritis. Ann Rheum Dis. 2022 Dec;81(12):1647-1653.
2) Dejaco C et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice: 2023 update. Ann Rheum Dis. 2024 May 15;83(6):741-751.
To cite this abstract in AMA style:
Matza M, Unizony S, Kohler M. Ultrasound Fast-Track Giant Cell Arteritis Clinic Experience in the United States [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/ultrasound-fast-track-giant-cell-arteritis-clinic-experience-in-the-united-states/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ultrasound-fast-track-giant-cell-arteritis-clinic-experience-in-the-united-states/