Session Information
Date: Sunday, November 13, 2016
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment I: Nephritis
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Tubulointerstitial damage (TID) is considered to be a later sequela of lupus nephritis (LN). The clinical significance of TID in patients with only mild to moderate renal impairment at the time of biopsy has not been studied. The objective of this study was to determine if TID predicts progression to end-stage renal disease (ESRD) in LN patients with mild to moderate renal impairment.
Methods: We identified all adult and pediatric SLE patients (by ACR and/or SLICC criteria) with who had an index biopsy consistent with LN (>6 glomerulai examined) between January 2005 and July 2015. Renal impairment was defined as mild (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73m2 ) or moderate (eGFR≥30 and <60 mL/min/1.73m2) at index biopsy. Demographic data, comorbidities, medications, laboratory data, ESRD onset, and deaths through December 2015 were ascertained from medical chart reviews, the United States Renal Data Systemic Report, and National Death Index. TID was defined as the presence of moderate to severe tubular atrophy and/or interstitial fibrosis as reported on the renal biopsies in accordance with the 2003 ISN/RPS criteria. Time to ESRD onset was defined as time from the index biopsy date to incident ESRD date; non-ESRD patients were censored at time of death or the last visit. Kaplan-Meier survival curves and Cox proportional hazards models were used to evaluate whether TID was predictive of ESRD progression adjusting for eGFR (as a continuous variable) and LN class.
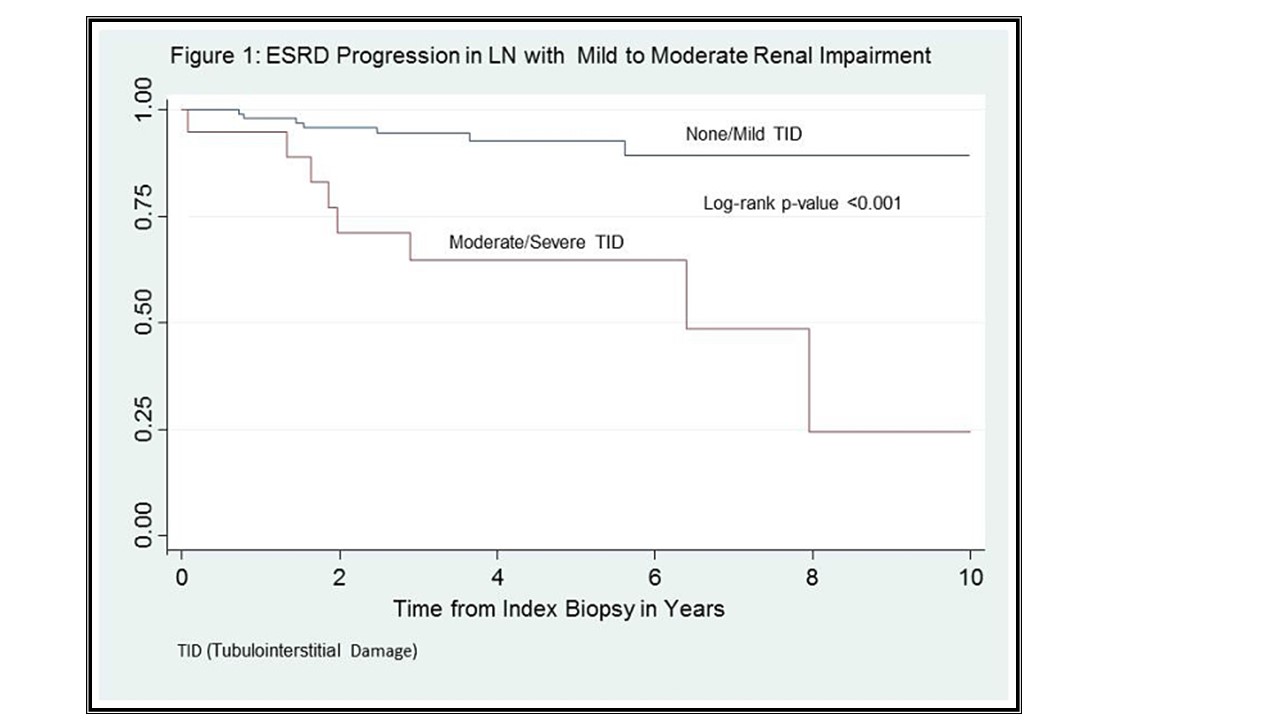
Results: Of the 155 patients with renal biopsies, 131 (85%) had baseline eGFR>30 mL/min/1.73m2: 8(6%) Class II, 58(44%) Class III/IV, 38(29%) Class V, and 27(21%) mixed; 16 (12%) progressed to ESRD. Eighty six percent of ESRD progressors had proliferative or mixed LN vs. 51% of non-ESRD, p=0.02. ESRD and non-ESRD groups were similar with respect to age, sex, race, comorbidity scores, complement levels, anti-dsDNA, and protein to creatinine ratio at index biopsy. Median (IQR) baseline eGFR was 65 (51, 75) mL/min/1.73m2 in the ESRD group and 97 (69, 127) mL/min/1.73m2 in the non-ESRD group, p=0.001. TID was present in 12% of biopsies with eGFR≥60 mL/min/1.73m2 and in 35% of biopsies with GFR between 30 and 60 mL/min/1.73m2. Moderate to severe TID was associated with a high risk of ESRD progression (Figure 1, log-rank p-value<0.001), HR=8.3, 95% CI: (2.6, 27), p-value<0.001, adjusted for eGFR and proliferative or mixed LN. Similarly, TID remained a significant predictor in the subgroup with eGFR>60 mL/min/1.73m2, HR= 5.6, 95% CI: (1.3, 22.9), p=0.02.
Conclusion: TID was highly prevalent among LN patients with mild to moderate renal impairment. TID was a strong predictor of ESRD progression in these patients independent of eGFR or biopsy class. Identifying factors associated with the presence of TID early in the disease may lead to the development of effective prevention strategies to decrease the risk of ESRD.
To cite this abstract in AMA style:
Jovanovic B, Khan HN, Mowrey W, Izmirly PM, Schwartz D, Buyon JP, Putterman C, Goilav B, Broder AR. Tubulointerstitial Damage Is an Independent Predictor of End Stage Renal Disease in Lupus Nephritis Patients with Mild to Moderate Renal Impairment [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/tubulointerstitial-damage-is-an-independent-predictor-of-end-stage-renal-disease-in-lupus-nephritis-patients-with-mild-to-moderate-renal-impairment/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tubulointerstitial-damage-is-an-independent-predictor-of-end-stage-renal-disease-in-lupus-nephritis-patients-with-mild-to-moderate-renal-impairment/