Session Information
Date: Sunday, November 8, 2015
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is associated with increased all-cause and cause-specific mortality, including mortality from cardiovascular (CV) disease, respiratory causes, infections and malignancy. Evidence of improved overall mortality in RA is growing and decrease in CV mortality has been suggested in some studies including our own. Recent trends in non-CV mortality are not well understood. We aimed to assess trends in non-CV mortality including mortality from respiratory disease, neoplasms and other causes in patients with incident RA in 2000-2007 compared to the previous decades.
Methods: The study population comprised a retrospectively identified population-based incidence cohort of patients with RA (age>18 years, 1987 ACR criteria met in 1980-2007). All subjects were followed until death, migration, or 1/1/2014. Underlying causes of death were obtained from state and local death certificates as well as the National Death Index Plus and grouped according to ICD-9 and ICD-10 chapters. Kaplan-Meier methods were used to estimate mortality rates. Cox proportional hazards models, adjusting for age and sex, were used to compare cause-specific mortality by decade.
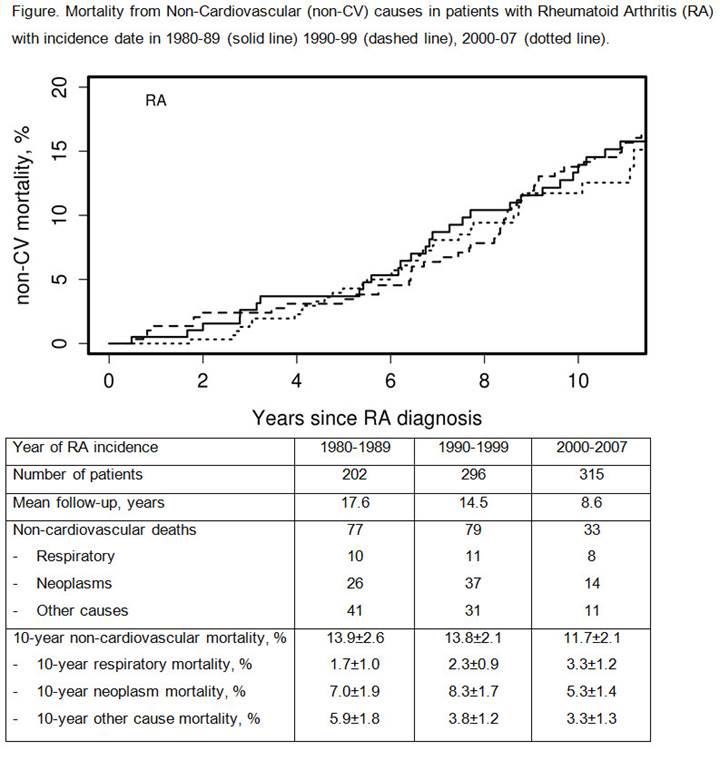
Results: The study included a total of 813 RA patients (mean age 55.9 years; 68% female; 66% rheumatoid factor [RF] positive). Figure shows non-CV mortality by decade of RA incidence and the table summarizes these data. In patients with incident RA during the 2000–2007 period, there was no statistically significant difference in 10-year mortality from non-CV causes overall (hazard ratio [HR] 0.92; 95% Confidence Interval [CI] 0.60 – 1.42; p=0.71), including mortality from respiratory disease (HR 1.51; 95% CI 0.56 – 4.09; p=0.42), neoplasms (HR 0.69; 95% CI 0.36 – 1.31; p=0.25) and other causes (HR 0.84; 95% CI 0.38 – 1.86; p=0.66) compared to those with RA incidence in 1990–1999.
Conclusion: Our findings suggest that there has been no significant improvement in mortality from non-CV causes overall among patients with incident RA in 2000-2007 compared to patients with incident RA in the previous decades. However, the trends in individual non-CV causes including respiratory disease, neoplasms and other causes may be heterogeneous and require caution in interpretation due to limited statistical power in our study. Lack of improvement in non-CV mortality in RA may be contributing to the persistent excess in relative mortality in RA vs non-RA subjects, suggesting a need for improved control of non-CV comorbidities in RA. More studies are needed to understand the underlying reasons for this lack of improvement in mortality from non-CV causes in RA patients.
To cite this abstract in AMA style:
Myasoedova E, Crowson CS, Matteson EL, Davis JM III, Gabriel SE. Trends in Non-Cardiovascular Mortality in Patients with Incident Rheumatoid Arthritis: Is There Room for Improvement? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/trends-in-non-cardiovascular-mortality-in-patients-with-incident-rheumatoid-arthritis-is-there-room-for-improvement/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-non-cardiovascular-mortality-in-patients-with-incident-rheumatoid-arthritis-is-there-room-for-improvement/