Session Information
Date: Monday, November 14, 2016
Title: Rheumatoid Arthritis – Clinical Aspects - Poster II: Co-morbidities and Complications
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
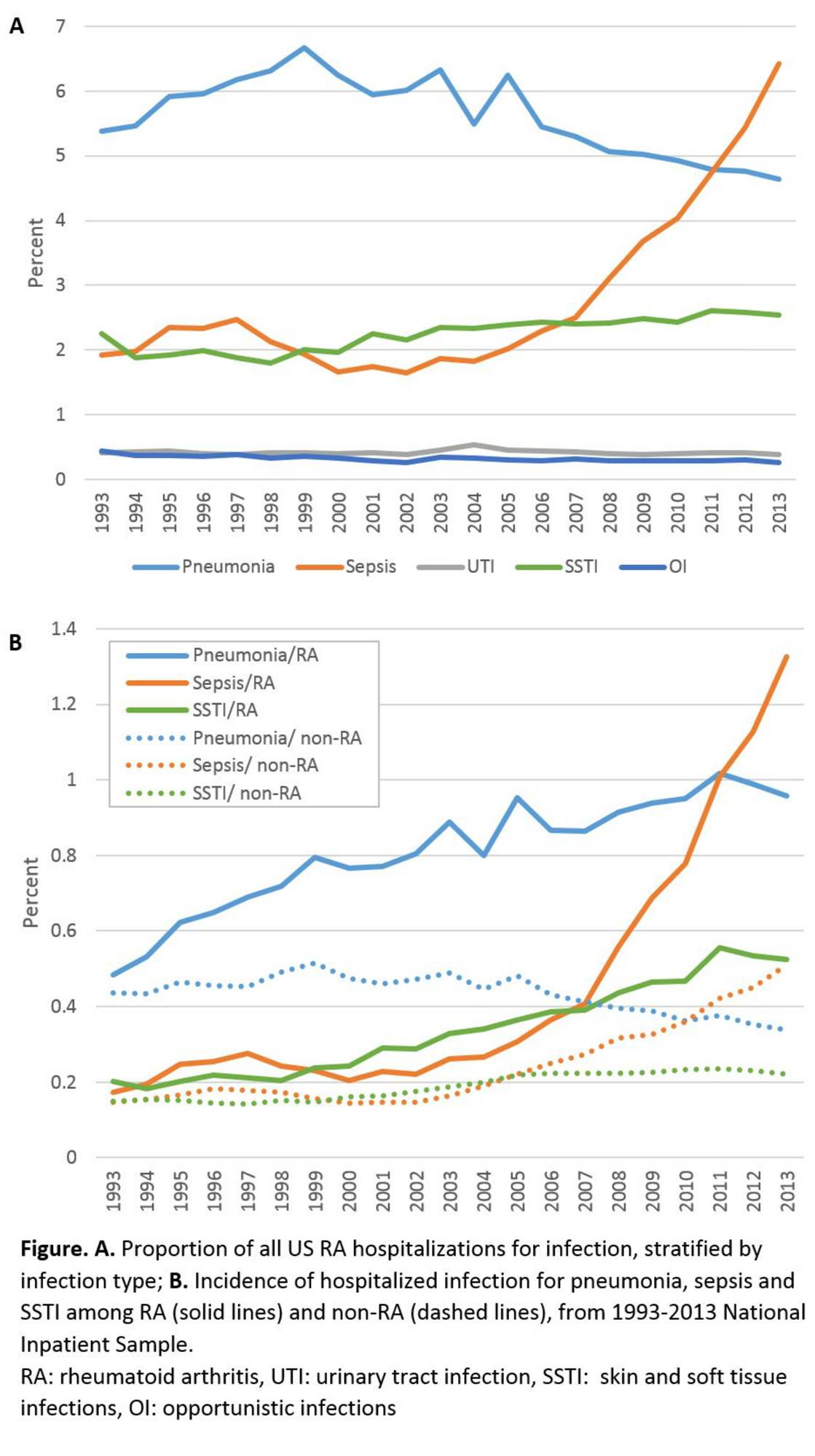
Methods: We conducted serial cross-sectional analyses of 1993-2013 data from the National Inpatient Sample, a nationally representative sample of all community hospitals in the US. We identified hospitalized adults with RA using an ICD-9 codes in any secondary diagnosis field. We evaluated 5 infections as the primary diagnosis: pneumonia, sepsis, urinary tract infection (UTI), skin and soft tissue infections (SSTI), and opportunistic infections (OI). The primary outcome was the proportion of hospitalizations for each infection, among all hospitalizations with a secondary diagnosis of RA. We considered the proportion of myocardial infarction (MI) hospitalizations among RA as a control condition, since reports indicate decreased incidence. We also calculated the incidence of each infection among RA patients by year, using an estimate of the national adult RA population as 1% of the adult US census population. The Cochran-Armitage Trend Test was used to examine trends.
Results: From 1993 to 2013 there were 792,921 hospitalizations for infection with a secondary diagnosis of RA. Hospitalizations with any secondary RA code increased from 60 to 160 per 100,000 persons (US general population). Among RA patients, the proportion of hospitalizations decreased for pneumonia (5.4 to 4.6%, p<0.001), UTI (0.42 to 0.38%, p=0.04), and OI (0.44 to 0.26% (p<0.001). The rate for SSTI increased slightly (2.3 to 2.5%, p<0.001), while the proportion of hospitalizations for sepsis more than tripled (1.9 to 6.4%, p<0.001). Consistent with previous reports, MI hospitalizations decreased from 2.2 to 1.8%. Using the theoretical national RA population as the denominator, without accounting for the increased RA coding over the study period, there appeared to be an increase in the rates of all infections: pneumonia (0.48 to 0.96%), UTI (0.37 to 0.79%), SSTI (0.20 to 0.52%), OI (0.039 to 0.055%) and sepsis (0.17 to 1.32%); all p values <0.001.
Conclusion: Between 1993 and 2013, the proportion of hospitalizations for infections among RA patients declined for pneumonia, UTI, and OI, with a small increase in the proportion for SSTI and a marked increase in sepsis. The sepsis results are consistent with previous reports that the sensitivity of sepsis coding has increased, but still warrant confirmation in other data sets such as RA cohorts. There has been a doubling of coding for RA in hospital discharges, which should be investigated further and acknowledged in studies using hospitalization data.
To cite this abstract in AMA style:
Jinno S, Lu N, Jafarzadeh SR, Dubreuil M. Trends in Hospitalizations for Infections in US Patients with Rheumatoid Arthritis, 1993-2013 [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/trends-in-hospitalizations-for-infections-in-us-patients-with-rheumatoid-arthritis-1993-2013/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-hospitalizations-for-infections-in-us-patients-with-rheumatoid-arthritis-1993-2013/