Session Information
Date: Tuesday, November 10, 2015
Title: Rheumatoid Arthritis - Small Molecules, Biologics and Gene Therapy Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Among rheumatoid arthritis (RA) patients who
progress beyond their first biologic disease-modifying antirheumatic drug (bDMARD),
in-class cycling between different tumor necrosis factor inhibitors (TNFi) has
been common practice. The introduction of newer bDMARDs targeting other
mechanisms of action (MOA) offer additional treatment options and could
introduce changes in clinical practice guidelines that directly impact
real-world clinical practice. This analysis aims to examine the trend of US RA
patients who switch bDMARD treatment following an initial TNFi, and to identify
patient and physician factors associated with switching to a bDMARD with a
different MOA rather than in-class cycling to a second TNFi.
Methods: Data were drawn from the Adelphi RA-DSP, a
cross-sectional geographically diverse survey of US rheumatologists about their
RA patients using samples from the 1st quarter (Q1) of 2011 and Q1
2014. Rheumatologists provided patient demographics, clinical details,
and treatment history. All patients had previously received a TNFi bDMARD as
their first bDMARD therapy. Patients who subsequently cycled in-class to a
second TNFi were compared to those switching to a bDMARD with a different MOA.
Multivariate analysis was performed to identify independent patient and
physician characteristics associated with switching to a bDMARD with a different
MOA as the second treatment strategy rather than in-class cycling to a second
TNFi.
Results: Included in the analysis were 246 RA patient cases that
had previously received a TNFi as their first bDMARD therapy and had progressed
onto a second bDMARD: mean age 56.0 years, 74.0% female, 83.1% RA-seropositive,
63.3% commercially insured, 25.3% Medicare, and 8.2% Medicaid. The main reasons
for discontinuing the first TNFi therapy included: loss of efficacy (55.2%),
lack of response (43.6%), adverse events (17.8%), and cost reasons (4.3%).
Comparing patient cases collected in 2011 and 2014, a significant
increase was observed in switching to bDMARDs with a different MOA (compared to
in-class cycling to a second TNFi), from 30% in 2011 to 43.1% in 2014 (P
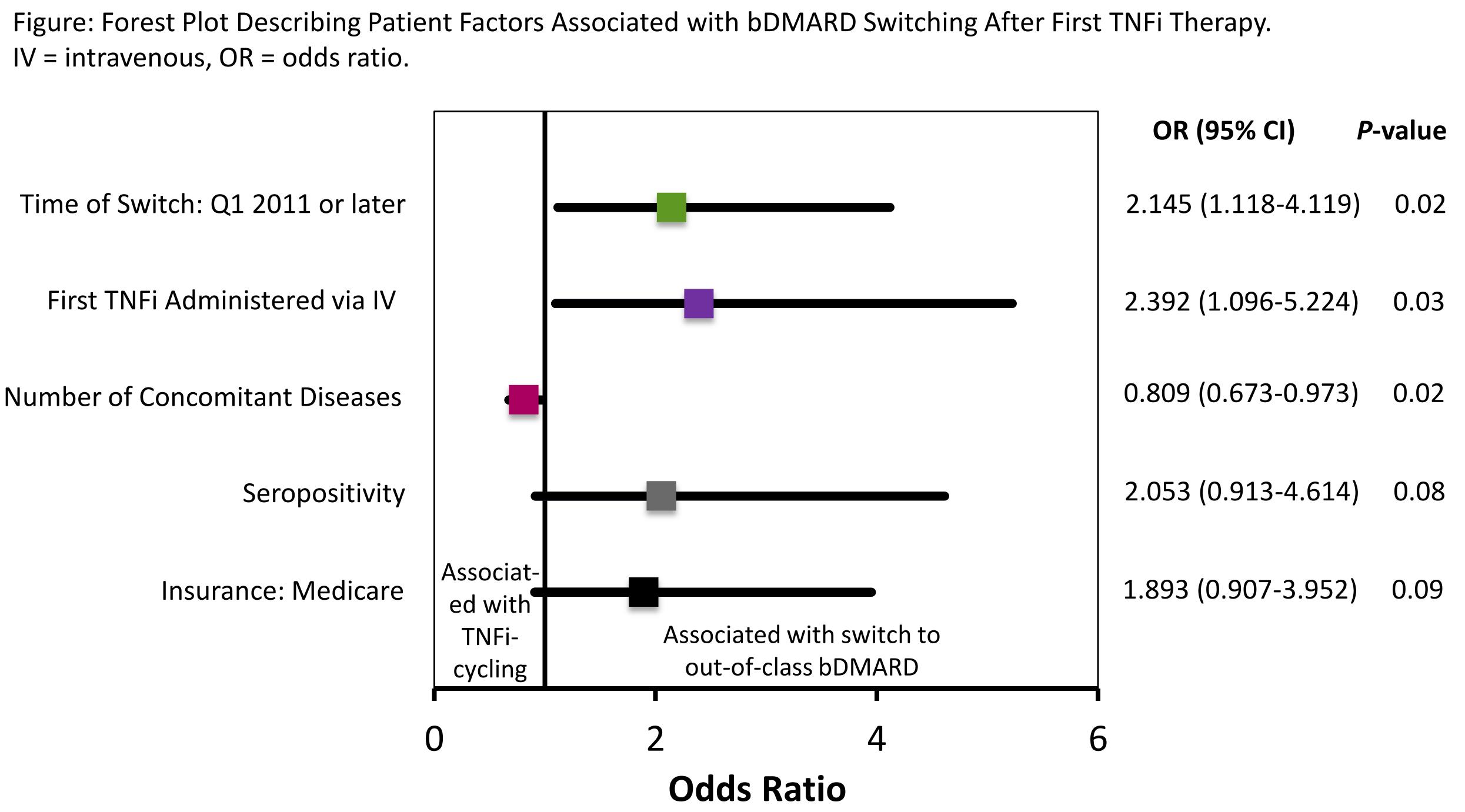
= 0.035). Multivariate analysis indicated that patients were more likely to
switch to a bDMARD with a different MOA if the switch occurred after Q1 2011
and if they had received their first line of TNFi intravenously, but less
likely to switch to bDMARDs with a different MOA when they had a high number of
concomitant conditions (Figure).
Conclusion: This study suggests that when switching between
bDMARDs occurred, US physicians increasingly switched their RA patients to a
bDMARD with a different MOA rather than in-class cycling to a second TNFi.
To cite this abstract in AMA style:
Wei W, Sullivan E, Chen CI, Piercy J, Blackburn S. Trend and Factors Associated with Switching Treatment after Initial Anti-TNF Therapy Among Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/trend-and-factors-associated-with-switching-treatment-after-initial-anti-tnf-therapy-among-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trend-and-factors-associated-with-switching-treatment-after-initial-anti-tnf-therapy-among-patients-with-rheumatoid-arthritis/