Session Information
Session Type: Abstract Session
Session Time: 2:00PM-2:15PM
Background/Purpose: Daily psychological stress and trauma exposure with or without symptoms of post-traumatic stress disorder have been linked to an increased risk of SLE onset.1, 2 Adverse childhood experiences (ACEs) have been linked to worse patient-reported outcomes in SLE, but not to physician-assessed disease activity.3 This analysis examines the association between experiences of trauma and disease flares in SLE.
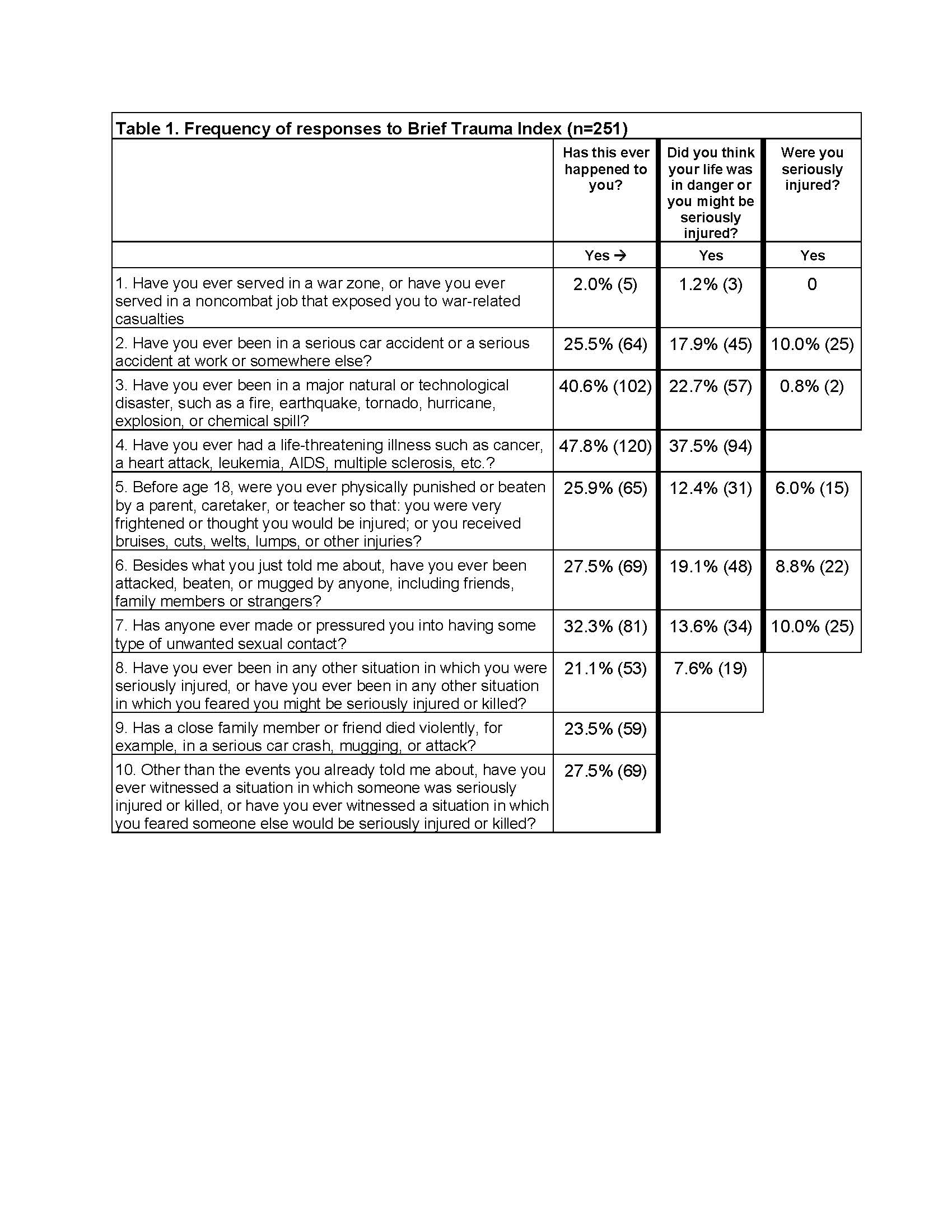
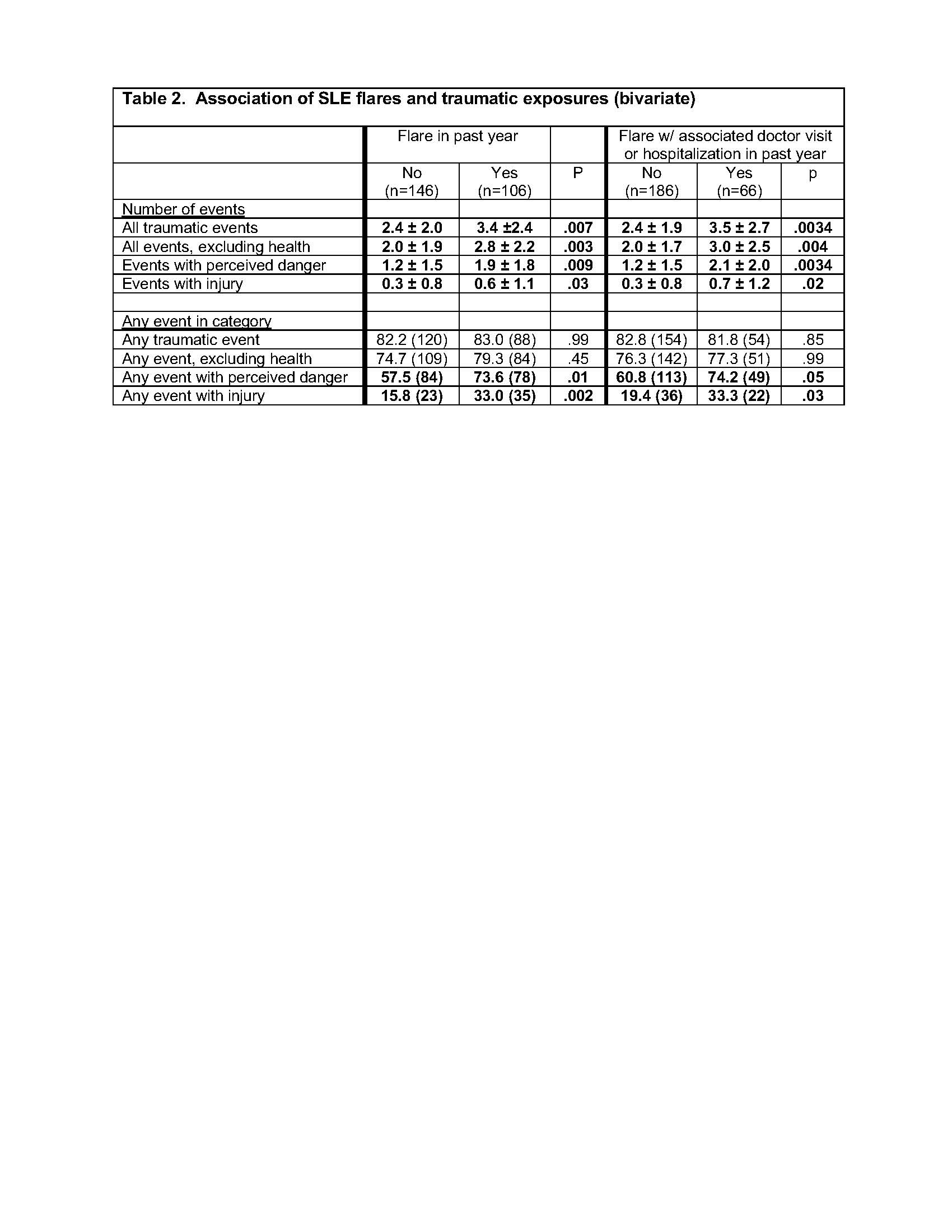
Methods: Data are from the California Lupus Epidemiology Study (CLUES), a longitudinal cohort of individuals with rheumatologist-confirmed SLE. Data are collected annually through in-person research visits and structured interviews. The Brief Trauma Index (BTI) was administered to assess the experience of trauma as well as whether the respondent believed they were at risk for serious injury or death, and whether they were actually injured (Table 1). In contrast to ACEs, traumatic events could be in childhood or adulthood, although one question specifically addresses childhood events. The total number of traumatic events, events with perceived danger, and events with injury, as well as the experience of any of these were calculated. Lupus flares over the previous year were self-reported as any flare (FLARE) or whether the respondent visited the doctor or was hospitalized for the flare (DR-FLARE). Cross-sectional analyses examined whether trauma (number of events or any event) was associated with flares. Multivariable analyses examined the role of trauma on the occurrence of flares controlling for age, disease duration, sex, poverty, race/ethnicity, comorbidities, and obesity. Finally, analyses were repeated and stratified by whether the individual reported ACEs. For this analysis, the BTI item on childhood trauma was excluded.
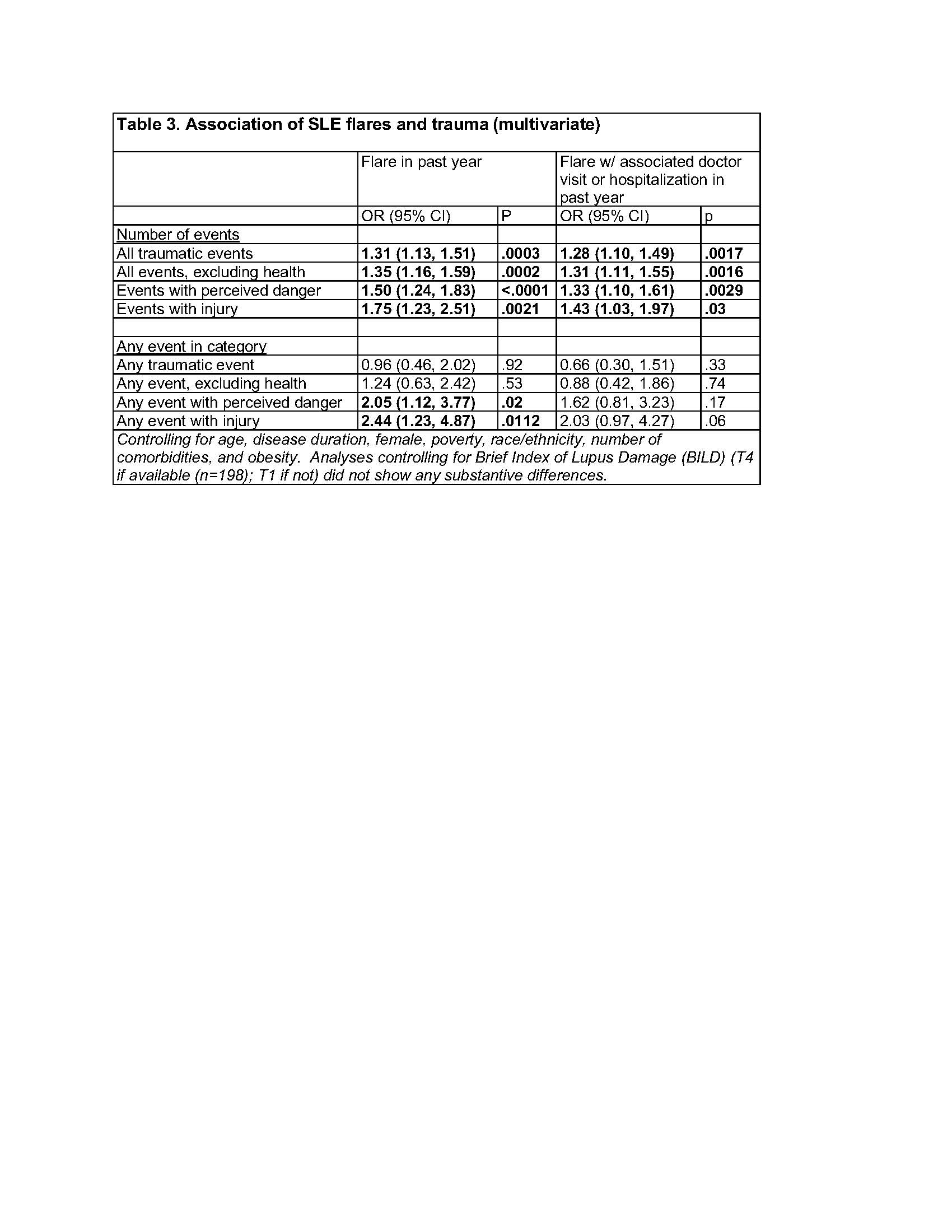
Results: Among the 251 individuals who completed the BTI, mean age was 50 ± 13 years, disease duration 22 ± 11 years, 90% were female, 31% Asian, 23% Hispanic, 33% white non-Hispanic, and 10% African American. 106 (42%) reported FLARE in the past year; 62% of these (n=66) reported DR-FLARE. 83% reported any trauma; excluding the BTI item on serious illness, 77% reported any trauma (Table 1). 64% reported trauma with perceived danger, and 23% with injury. Among those with FLARE and DR-FLARE, the number of all types of events was higher (Table 2). In multivariate analyses, the associations remained significant (Table 3). The association between trauma in adulthood and flares appeared to be stronger among individuals who had previously experienced ACEs (e.g., 0-1 ACEs, odds of DR-FLARE per number of traumatic events = 1.2 [95% CI 0.9, 1.6)] vs. ≥2 ACES 1.7 [1.2, 2.5]).
Conclusion: Individuals with SLE who have experienced trauma during adulthood may be at increased risk for more frequent self-reported flares over time, and the experience of childhood trauma may magnify that risk. Given the high frequency of traumatic experiences, identifying both the mechanisms of these associations and interventions that may reduce the impact of trauma is critical.
1. Roberts A, et al. Arthritis Rheum. 2017;69:2162-2169.
2. Feldman CH, et al. J Rheumatol. 2019;46(12):1589-1596.
3. DeQuattro K, et al. Arthritis Care Res. 2020;72(525-533).
To cite this abstract in AMA style:
Katz P, DeQuattro K, Patterson S, Trupin L, Barbour K, Rush S, Lanata C, Yazdany J, Dall'Era M. Trauma Is Associated with Flares in Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/trauma-is-associated-with-flares-in-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trauma-is-associated-with-flares-in-systemic-lupus-erythematosus-sle/