Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Thursday, April 30, 2020
Title: Poster Session 1
Session Type: ACR Abstract Session
Session Time: 6:00PM-7:00PM
Background/Purpose: The transition from pediatric to adult rheumatology is linked to poor outcomes in the absence of comprehensive transition programs. Several tools are available to measure transition readiness. Transition success is influenced by patient age and family history of disease, yet little is known about the impact of patient-provider relationship on transition readiness.
In our multidisciplinary transition clinic, adolescents (14-18 years) with childhood-onset Systemic Lupus Erythematosus (cSLE) or Juvenile Idiopathic Arthritis (JIA) are seen by pediatric and adult rheumatologists concurrently, along with a nurse, child life specialist and physiotherapist with advanced rheumatology training. An adult rheumatologist also runs a young adult clinic for patients 18 to 25 years old. We evaluated (1) readiness for transition among patients with JIA and cSLE, (2) patients’ perceptions of the patient-provider relationship, and (3) the potential association between these factors.
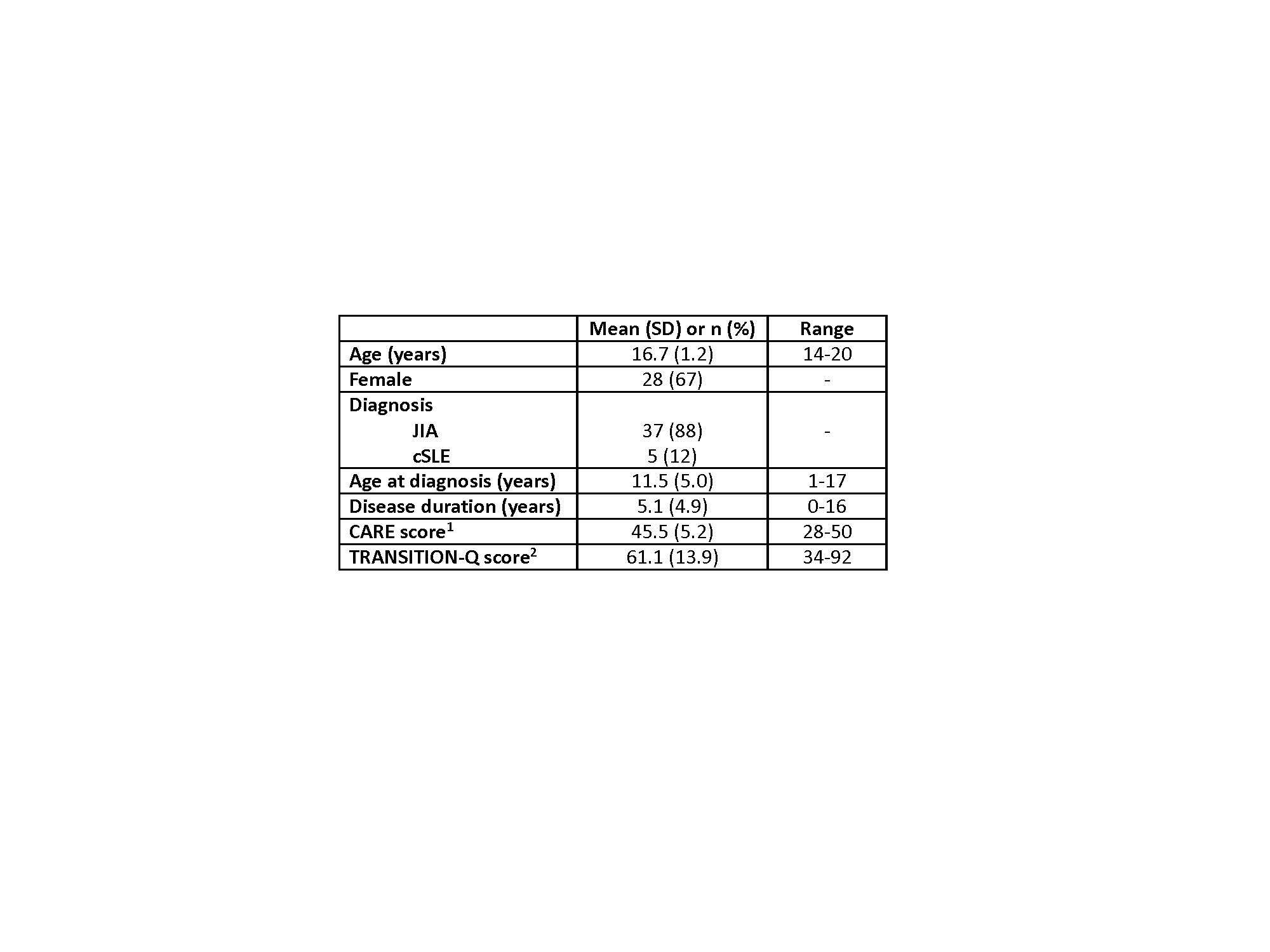
Methods: Patients with cSLE or JIA were recruited from the transition and young adult clinics at a single academic institution. Participants completed the Consultation and Relational Empathy Scale (CARE) questionnaire (10-items, max 50) which evaluates patients’ perception of physicians’ care and empathy on a 5-point Likert scale (poor-excellent) and the TRANSITION-Q, a validated 14-item questionnaire (max 100) which assesses healthcare self-management skills as a proxy for transition readiness. Descriptive statistics summarized patient characteristics and questionnaire scores. Multivariable linear regression analyses determined the association between age and disease duration and each of the CARE and TRANSITION-Q scores. We repeated the analysis with CARE scores to determine the potential effect of the parent-provider relationship on TRANSITION-Q scores.
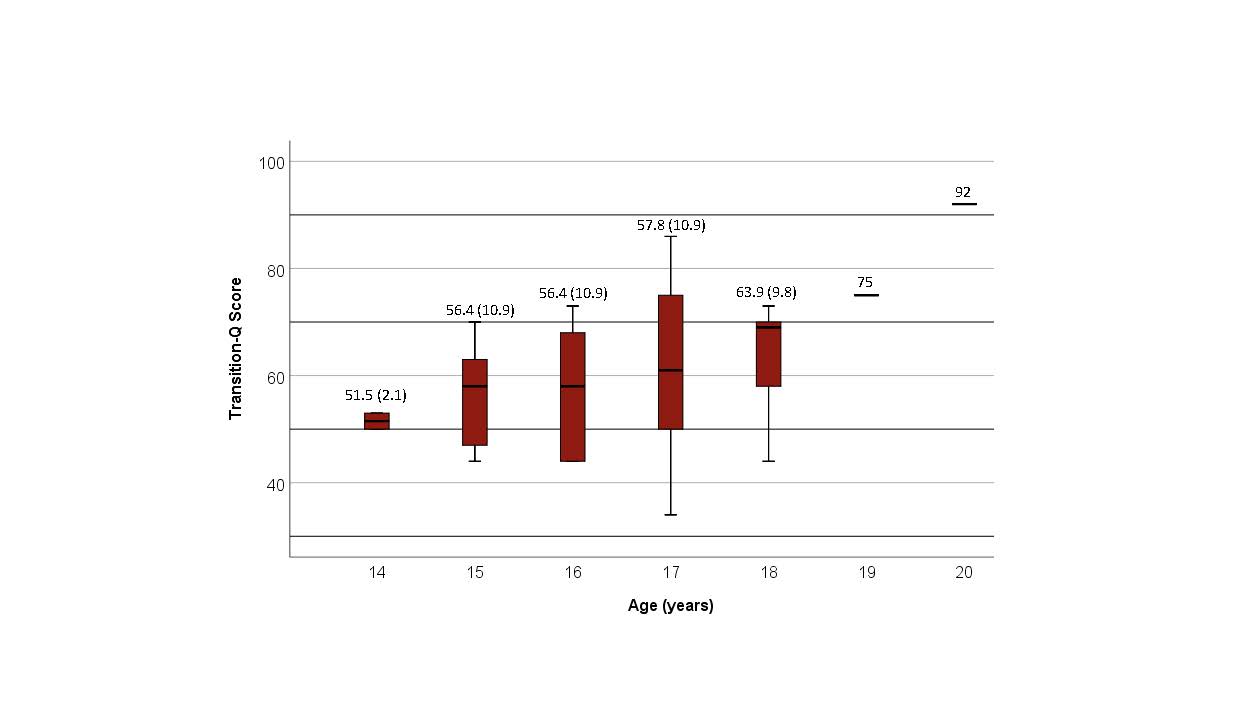
Results: Characteristics of the 42 participants are shown in Table 1. Mean TRANSITION-Q scores increased with age (Figure 1). Age, but not disease duration, was significantly associated with TRANSITION-Q (standardized β =0.385, p=0.019) and CARE scores (standardized β =0.414, p=0.011). CARE scores were overwhelmingly positive with 71% scoring ≥ 45. While CARE and TRANSITION-Q scores appeared positively correlated (r= 0.33, p=0.04), the model examining the association between CARE and TRANSITION-Q scores accounting for age and age at diagnosis revealed only age was significantly associated with TRANSITION-Q scores (adjusted R2=0.13, p=0.02). This suggests that age is the primary driver of the association between TRANSITION-Q and CARE.
Conclusion: Readiness for transition from pediatric to adult rheumatology appears to increase with patient age. Favorable perceptions of the patient-provider relationship also increase with patient age, yet these do not appear to impact transition readiness beyond age itself. While our results suggest that interventions to improve transition readiness should focus on the improvement of self-management skills and not on the patient-provider relationship, the lack of variability in CARE scores limits our ability to draw definitive conclusions about the impact of the patient-provider relationship on transition readiness.
1.Maximum possible CARE Score is 50; 2.Maximum possible TRANSITION_Q score is 100.
To cite this abstract in AMA style:
Semalulu T, Beattie K, McColl J, Alam A, Thomas S, Herrington J, Gorter J, Cellucci T, Garner S, Heale L, Matsos M, Batthish M. Transition from Pediatric to Adult Rheumatology: The Clinician as a Fundamental Ally [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/transition-from-pediatric-to-adult-rheumatology-the-clinician-as-a-fundamental-ally/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/transition-from-pediatric-to-adult-rheumatology-the-clinician-as-a-fundamental-ally/